This website is intended for healthcare professionals only.
Take a look at a selection of our recent media coverage:
7th November 2024
An ‘early warning system’ for future pandemics is to be rolled out in the UK to monitor threats, prevent disease and protect the public, the Department of Health and Social Care (DHSC) has announced.
The surveillance system will be created via the expansion of NHS England’s respiratory metagenomics programme, led by Guys and St Thomas’ NHS Foundation Trust. It uses technology created by life sciences company Oxford Nanopore to analyse genes and pathogens to rapidly diagnose cancers and rare and infectious diseases and match patients with the right treatments within six hours.
The expansion of the programme will also allow potential outbreaks of bacterial or viral diseases to be monitored across the country, alongside antimicrobial resistance.
The technology was initially piloted at St Thomas’ hospital and will be rolled out across 30 NHS sites. Data will be given to the UK Health and Security Agency to allow for quicker detection and action on emerging infectious diseases.
The programme is a partnership between the government, Genomics England, UK Biobank, NHS England and Oxford Nanopore.
Health secretary Wes Streeting said: ‘If we fail to prepare, we should prepare to fail. Our NHS was already on its knees when the pandemic struck, and it was hit harder than any other comparable healthcare system.
‘We cannot let history repeat itself. That’s why this historic partnership with Oxford Nanopore will ensure our world-leading scientists have the latest information on emerging threats at their fingertips.’
Professor Dame Sue Hill, chief scientific officer for England, said: ‘This strategic partnership will build upon our expertise in infectious disease genomics, representing a significant leap forward in our ability to protect public health and save lives.
‘By integrating cutting-edge technology into 30 NHS sites across the country, we are not only enhancing our capacity to rapidly diagnose and treat severe respiratory infections, but also creating a crucial early warning system for new and emerging infectious diseases.’
Professor Susan Hopkins, chief medical advisor at the UK Health Security Agency, said: ‘Enhancing the capacity for the NHS to determine new and emerging pathogens causing severe acute respiratory infections will improve the detection and emergence of infections.
‘As part of the 100 days mission, this will enable the development of effective diagnostics for novel pathogens and enhance our pandemic preparedness.‘
Professor Ian Abbs, chief executive of Guy’s and St Thomas’ NHS Foundation Trust, said: ‘We’ve been working on the respiratory metagenomics programme for over four years and have clearly seen the benefit to our patients. It’s a momentous day now that we can ensure other hospitals, and more patients, can also benefit from faster and more accurate treatment for severe respiratory conditions thanks to new genomic technology.’
A version of this article was originally published by our sister title Healthcare Leader.
21st June 2024
The Covid-19 pandemic profoundly impacted global health and fundamentally altered our comprehension of infectious diseases and pandemic control. Amidst the spotlight on vaccine development, therapeutic interventions remained a critical, yet often overlooked, aspect of pandemic preparedness. Here, Gerry Hughes explores the importance of therapeutic technologies for future pandemics and the pathogens and candidate therapies that clinicians should take note of.
The Covid-19 pandemic catalysed a rapid advancement in our understanding of viral infections, yielding valuable insights on managing a modern-age pandemic. While the concept of medical countermeasures encompassing diagnostic, preventative and treatment interventions for public health emergencies is not novel, the pandemic brought it back sharply into focus.
Early in the pandemic, decades of preceding research on messenger Ribonucleic Acid (mRNA) vaccines expedited the development of Covid-19 vaccine technologies, and repurposed drugs like dexamethasone and tocilizumab proved effective in treating hospitalised Covid-19 patients.
However, identifying evidence-based therapeutics posed challenges. Agents such as hydroxychloroquine and lopinavir/ritonavir, initially promising, yielded unsatisfactory results in clinical trials, and remdesivir demonstrated limited efficacy. Newer drugs such as molnupiravir and nirmatrelvir wouldn’t emerge as therapeutic options until later in the pandemic, and they remain prohibitively expensive in many cases.
These shortcomings in Covid-19 therapeutics were discussed at a recent virtual panel discussion entitled ‘Fair Treatment: The Place of Therapeutics in Future Pandemics’. Professor Sharon Lewin, director of the Cumming Global Centre for Pandemic Therapeutics (CGCPT) at the Peter Doherty Institute for Infection and Immunity, summarised that Covid-19 therapeutics ‘came too late, they weren’t fantastic drugs, and they weren’t equitably available across the world’.
Eloise Todd, executive director and co-founder of the Pandemic Action Network, pointed out that loose governance of international efforts to rapidly develop therapeutics during the Covid-19 pandemic left the therapeutics landscape lagging behind the ‘vaccines goldrush’.
According to the CGCPT, if nirmatrelvir plus ritonavir or molnupiravir ’had been available at scale in July 2020, in line with Covid-19 vaccine approval, it could have prevented millions of deaths globally’.
Recognising the need to better prepare for a future pandemic, the World Health Organization (WHO) is currently leading the charge in developing a global pandemic accord – a framework to help prevent future health emergencies and for countries to adequately respond to any that do emerge.
To achieve this, governmental leaders from 194 countries are currently negotiating the terms of the accord, which involves collating and analysing scientific evidence regarding the potential triggers of future pandemics. Despite ongoing discussions and the intention to finalise the terms at the 77th World Health Assembly held in Geneva earlier this year (27 May – 1 June 2024), a final text remains elusive.
While a new set of international health regulations were agreed at the Assembly, the timeline for the terms of the pandemic accord was extended to the next meeting in 2025.
In its 2023 technical report on the Covid-19 pandemic in the UK, the Department of Health and Social Care described critical lessons learned. It highlighted that emphasis on collaborative partnerships among the National Health Service, funders, academia, the pharmaceutical industry and the general public played a pivotal role in shaping effective pandemic management. This cross-sector collaboration facilitated several impactful strategies:
Looking ahead, the success of Covid-19 vaccination programmes may not be fully replicable in future pandemics. This is because the accelerated vaccine response owed much to decades of prior mRNA research – a unique advantage that may not recur. In such a situation, the availability of safe and effective therapeutics becomes critical.
Professor Michel Kazatchkine, another ‘Fair Treatment’ panellist and a physician and professor of immunology at the Paris Descartes University, France, emphasised the importance of partnering therapeutics with vaccines, not only to improve patient outcomes but to reduce onward infection transmission.
For example, valuable experience was gained from the use of monoclonal antibodies (mAbs) during Covid-19. This experience indicates that mAbs may be best targeted towards diagnostically confirmed disease, increasing disease severity, unvaccinated populations and where the local healthcare system can support delivery of these agents.
Earlier this month, the Independent Panel for Pandemic Preparedness and Response recommended a strategic shift to better align prevention and treatment interventions for deployment in a subsequent pandemic.
The authors noted that during Covid-19, vaccines were ‘one of several tools required to contain a public health emergency, and investment in diagnostics and treatments must also be commensurate’, but the ‘dominant focus on vaccines’ meant ’progress on diagnostics and treatments has been meagre, despite their importance as a first line of response’.
In a study published earlier this year, 187 infectious disease experts from 57 countries answered a survey to rank various pathogens based on their perceived risk of causing a future pandemic. Results from that study showed that experts were most concerned about influenza, severe-acute-respiratory-syndrome coronavirus (SARS-CoV), SARS-CoV-2 and Ebola.
The Coalition for Epidemic Preparedness Innovations (CEPI) – a global partnership working to accelerate the development of vaccines and other biologic countermeasures against epidemic and pandemic threats – has also raised concerns about several other diseases, namely: Chikungunya, Lassa Fever, Middle East Respiratory Syndrome (commonly known as MERS), Nipah and Rift Valley Fever.
More concerning, perhaps, are novel viral threats with epidemic or pandemic potential that have not yet been characterised – otherwise known as ‘Disease X’. This hypothetical disease exhibits several key features: a viral, zoonotic and mutated pathogen transmitted via respiratory aerosols or droplets.
The International Readiness for Preventing Infectious Viral Disease (INTREPID) Alliance is a non-profit consortium of innovative biopharmaceutical companies dedicated to accelerating the pipeline of antiviral treatments to help protect the world ahead of future pandemics. Part of their mission is to accelerate the collective understanding of antiviral research and development by identifying promising clinical and preclinical compounds.
In April 2024, the INTREPID Alliance published an updated review of antiviral compounds in clinical development for 12 priority virus families of pandemic potential. Of 41 compounds at various phases of clinical development, the INTREPID Alliance has identified 11 of these (see Table 1) as showing promise in fulfilling a ‘100 Days Mission Ready’ brief.
The goal of the 100 Days Mission is to prepare as much as possible so that within the first 100 days of a pandemic threat being identified, key therapeutic interventions can be made available in a safe, effective and affordable way.
3CLPRO is a popular drug target given that its enzymatic activity is critical for the formation of functional viral proteins during viral replication. Almost all the other targets described in Table 1 are enzymes important for functional viruses.
Table 1: 100-Day Mission Ready antiviral compounds in clinical development*
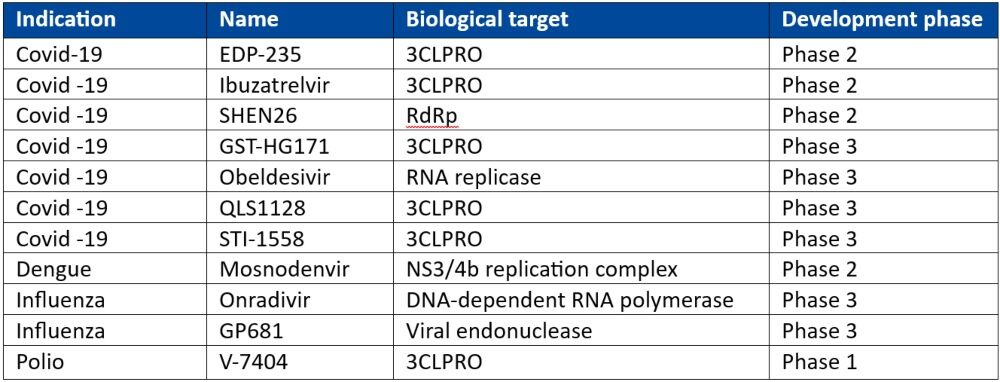
3CLPRO: 3C-like Protease; DNA: deoxyribonucleic acid; RdRp: RNA-dependent RNA polymerase; RNA: ribonucleic acid
*Adapted from the INTREPID alliance Antiviral Clinical Development Landscape – Second Edition
In their closing remarks during the Fair Treatment panel, speakers underscored the intricate challenge of balancing prevention and treatment strategies for the next pandemic. For example, one strategy may involve the use of the aforementioned mAb technology to potentially confer immediate immunity to disease while awaiting a vaccine response. Equally crucial is ensuring equitable access to these interventions.
Strategic investment will play a pivotal role in navigating these challenges, but clinicians and researchers can also play an important part in pandemic preparedness by becoming more engaged with research and development platforms.
Much of the work being undertaken explores emerging approaches – such as gene editing and gene silencing – to directly target pathogen genetic code with the aim of enhancing the innate immune response against entire virus families. Developing cost-effective, broadly active biologics such as antibodies is also a key focus.
What’s more, while it’s not expected as a panacea, the anticipated global pandemic accord agreement within the next 12 months will hopefully provide a robust platform for future-proofing another pandemic, including strategies for improved therapeutic preparedness.
2nd April 2024
The number of years people are expected to life in good health has fallen in both men and women, likely due to the Covid-19 pandemic, according to Office of National Statistics (ONS) figures.
Between 2011-13 and 2020-22, healthy life expectancy fell by 9.3 months to 62.4 years in males and by 14 months to 62.7 years in females. However, there were minimal changes up to 2017-19. This meant it was ‘likely the coronavirus (Covid-19) pandemic contributed to this decrease’, the ONS said.
The largest drop for male healthy life expectancy in England was in the north east, with a decrease of 20.3 months. For females, the area with the greatest reduction was the east Midlands (31.8 months).
Senior fellow at The King’s Fund, Veena Raleigh, said the latest data provides ‘graphic’ evidence of the declining state of people’s health in England.
‘As there had been minimal change in healthy life expectancy up to 2017-19, it’s likely that the pandemic in 2020 will have contributed to this fall. It’s also likely that the delays in care for non-Covid conditions and an increase in long-term sickness following the pandemic will have been contributory factors,’ she said.
Earlier this year, ONS figures showed that overall life expectancy in 2020-22 had fallen for males and females, to 78.8 and 82.8 years respectively.
‘So not only has life expectancy stalled, but more years are now spent in poor health. Currently, males and females spend almost one-quarter of their lives in poor health,’ Ms Raleigh added.
Commenting on the ’extremely concerning’ data, Dr Sarah Clarke, president of the Royal College of Physicians, said: ’The fact that people in some parts of the country have six more years of healthy life than others highlights the urgent need to address health inequalities.
’To narrow this gap we need to tackle the factors that make people ill in the first place – from poor housing, air quality, and the marketing of food and alcohol, to employment (including how much money you have), racism and discrimination, and transport.’
As such, Dr Clarke called for ‘coordinated and collective efforts from all parts of Government‘.
She said: ‘The Government’s upcoming Major Conditions Strategy – which the Secretary of State for Health and Social Care said this week [26 March] would be published over the next few months – is a vital opportunity to commit to bold cross-Government action. Without concerted action from across government, ill health in the population is likely to grow.‘
Ms Raleigh echoed this, calling for ‘bolder measures’ to prevent and manage ill health to be an ‘urgent priority’ for the Government.
A version of this article was originally published by our sister publication Healthcare Leader.
9th February 2024
Reduced pollution levels and better air quality during the Covid-19 pandemic lockdowns strongly correlated with lower rates of acute asthma care provision, according to new research led by the University of Birmingham.
The retrospective time-series study, published in the BMJ Open, investigated the link between acute asthma hospital admissions and specific air pollutant levels in four Oxford postcodes during the national lockdowns of March to June and November to December 2020.
For adult residents, acute asthma admissions fell from 78 per 100,000 residents in 2015-19, to 46 per 100,000 residents in 2020 – a reduction of 41%.
This reduction in acute asthma care coincided with levels of air pollution falling significantly. Different pollutants dropped by 18-33% when compared to average values for the previous five-year period.
For example, nitrogen dioxide (NO2) reduced by 26.7% from a 2015-19 average of 14.6 μg m-3 to 10.7 μg m-3 in 2020.
Fine particulate matter (PM2.5) saw a reduction of 33.5% from 10.1 μg m-3 in 2015-19 to 6.7 μg m-3 in 2020, and PM10 reduced by 18.6% from 13.2 μg m-3 in 2015-19 to 10.8 μg m-3 in 2020.
‘Large-scale measures to improve air quality have potential to protect vulnerable people living with chronic asthma in urban areas,’ the authors concluded.
Commenting on the ‘unique situation’ of temporary air quality improvement, Dr Suzanne Bartington, clinical associate professor of environmental health at the University of Birmingham and lead author of the study, said: ‘The results of air pollution levels falling may have had an impact on the number of severe asthma cases that need acute hospital care, with 41% fewer hospital stays compared to the previous five-year average.
‘Furthermore, we also identified a 4% increase in risk of asthma hospital admissions for every 1 μg m-3 increase in mean monthly NO2, and an approximately 3% increase in risk for every 1 μg m-3 increase in mean monthly PM2.5 levels.
‘This is an important study to help us better understand how demand for NHS inpatient care may change when air quality is improved.’
The research team was supported by the University of Oxford, Oxfordshire County and City Councils and the then Oxfordshire Clinical Commissioning Group.
Commenting on the results, Councillor Nathan Ley, Oxfordshire County Council’s cabinet member for public health, inequalities and community safety, said: ‘We must now use what we have learned, thanks to this research with our partners, to improve our environment, in line with the Clean Air Strategy which we launched last year.
‘Elevated levels of NO2, PM2.5 and PM10 contribute towards heart disease, chronic lung disease, cancers, preterm births, and many other avoidable events. The vision of Oxfordshire County Council to tackle this issue remains clear. We must continue to use all the tools at our disposal to lead the country, clean up our air and save lives.’
Earlier this week, the European Respiratory Society (ERS) warned of rising respiratory diseases, such as asthma, as well as premature death without urgent action on air quality.
This followed the ERS consensus statement on climate change and respiratory health, published in September 2023, which highlighted the damaging effects of air pollution on health and global warming.
8th November 2023
There was a more rapid cognitive decline in people aged over-50 during the pandemic, according to recent research, highlighting the need for public health measures to protect against dementia risk.
Covid-19 infection was found to be a risk factor, but the general more rapid decline in brain health was apparent even if people had not had the virus, the researchers found.
Published in the journal The Lancet Healthy Longevity, the online PROTECT study found a 50% change in the rate of cognitive decline in the first year of the pandemic among the 3,000 participants.
The analysis of tests of short-term memory and complex tasks also found that the rate of cognitive decline was higher in those who already had mild cognitive decline before the pandemic.
It appears to have been exacerbated by a number of factors among the 50-to-90-year-olds taking part, including an increase in loneliness and depression, a decrease in exercise and higher alcohol consumption.
In the second year of the pandemic, reduced exercise continued to affect executive function and associations were sustained between worsening working memory and increased alcohol use. This suggested a sustained impact after the initial 12-month period of lockdowns, the team from the University of Exeter and King’s College London (KCL) said.
The sustained drop in cognition highlights the need for public health interventions to mitigate the risk of dementia – particularly in people with mild cognitive impairment where diagnosis of dementia within five years is a substantial risk, they concluded.
Professor Anne Corbett, professor of dementia research and the PROTECT study lead at the University of Exeter, said: ‘Our findings suggest that lockdowns and other restrictions we experienced during the pandemic have had a real lasting impact on brain health in people aged 50 or over, even after the lockdowns ended.
‘This raises the important question of whether people are at a potentially higher risk of cognitive decline which can lead to dementia.
‘It is now more important than ever to make sure we are supporting people with early cognitive decline, especially because there are things they can do to reduce their risk of dementia later on.’
She added that the findings highlight the need for policymakers to consider the wider health impacts of restrictions like lockdowns when planning future pandemic responses.
Professor Dar Aarsland, professor of old age psychiatry at KCL, said the research adds to the knowledge of the long-standing health consequences of Covid-19, particularly for the most vulnerable people such as older people with mild memory problems.
He said: ‘We know a great deal of the risks for further decline, and now can add Covid-19 to this list. On the positive note, there is evidence that lifestyle changes and improved health management can positively influence mental functioning. The current study underlines the importance of careful monitoring of people at risk during major events such as the pandemic.’
A version of this article was first published by our sister publication Pulse.
9th May 2023
The global health emergency posed by Covid-19 is over, the World Health Organization (WHO) has declared, while also stressing that the disease remains a ‘global health threat’.
For over a year, the Covid-19 pandemic had been ‘on a downward trend’, due to population immunity increasing from vaccination and infection, mortality decreasing and the pressure on health systems easing, said Dr Tedros Adhanom Ghebreyesus, director-general of the WHO.
WHO and the Emergency Committee, convened under the International Health Regulations, ‘have been analysing the data carefully and considering when the time would be right to lower the level of alarm’ over the last twelve months.
Based on their recommendations, Dr Tedros declared Covid-19 over as a global health emergency on 5 Mya 2023, making the statement ‘with great hope’ he said.
‘That does not mean Covid-19 is over as a global health threat’, he stressed. Indeed, one person dies from Covid-19 every three minutes, thousands of people around the world are currently in intensive care units with the condition and there are ‘millions more’ suffering the effects of long-Covid.
‘This virus is here to stay. It is still killing, and it’s still changing. The risk remains of new variants emerging that cause new surges in cases and deaths,’ Dr Tedros said, warning countries to be complacent. ‘The worst thing any country could do now’ would be ‘to use this news as a reason to let down its guard, to dismantle the systems it has built, or to send the message to its people that Covid-19 is nothing to worry about’.
Instead, he advised countries to transition from ’emergency mode to managing Covid-19 alongside other infectious diseases’,’ added Dr Tedros’, evidence of which has been seen recently with WHO’s recent pulse survey revealing a move towards restoring essential health services.
Dr Tedros also celebrated the efforts of healthcare workers in helping to control the virus.
‘We have arrived at this moment thanks to the incredible skill and selfless dedication of health and care workers,’ he said. ‘The suffering we have endured, the painful lessons we have learned, the investments we have made and the capacities we have built must not go to waste’.
‘We owe it to those we have lost to leverage those investments; to build on those capacities; to learn those lessons, and to transform that suffering into meaningful and lasting change,’ he added, urging ‘a commitment to future generations that we will not go back to the old cycle of panic and neglect that left our world vulnerable’.
A version of this story was originally published by our sister publication The Pharmacist.
19th November 2021
The level of cancer diagnoses in young people fell during the first-wave of the COVID-19 pandemic but there was also an increased likelihood of admission to intensive for cancers diagnosed during the period. This was the finding from a study by researchers from Oxford University, UK who discussed their findings in a poster presentation at the National Cancer Research Institute conference.
The COVID-19 pandemic has had a major impact on cancer services in the majority of countries across the world. In the UK, a survey by Cancer Research UK in July 2020, found that 2 in 3 cancer patients reported that their cancer care had been impacted and that ratings of overall cancer care as ‘very good’ decreased from 75% ‘before lockdown started’ to 37% ‘after lockdown started’. Moreover, other research shows that in England, there were approximately 3.4 million fewer key diagnostic tests performed between March and August 2020 compared with the same period in 2019.
Given the likely impact of delays in diagnostics, the Oxford team were interested in determining how in England, the first wave of the pandemic affected childhood, teenager and young adult cancer incidence rates, diagnostic and treatment time-intervals and cancer-related intensive care (ICU) admissions. They used the QResearch database, which is derived from the anonymised health records of over 35 million patients. In addition, since QReseaerch is also linked to linked to hospital admission, mortality and cancer diagnoses data held with a disease register, it was possible for the researchers to make links between these three factors. For the present study, researchers focused on central nervous system (CNS) tumours, lymphomas, leukaemias, sarcomas and renal tumours in those aged up to 25 years of age. They compared the incidence of these cancer diagnoses between 1st February to the 15th August 2020 and compared their findings to the three preceding pre-pandemic years. As well as the number of diagnoses, the team also analysed the length of time before treatment started after diagnosis and whether or not these patients were diagnosed after being admitted to intensive care.
Findings
A total of 2607 cancer diagnoses were made from 1st January 2017-15th August 2020, with 380 during the pandemic. Overall, this represented a 17% reduction (95% CI -38% to – 6%) in the incidence-rate-ratio during the first wave of the pandemic. In particular there was a 38% (95% CI -52% to -21%)] decrease in CNS tumours and a 28% (95% CI -45% to -5%) reduction in lymphomas. Interestingly, the researchers observed that childhood cancers that were diagnosed during the pandemic were more than twice as likely to be associated with an ICU admissions (adjusted odd ratio, OR = 2.2, 95% CI 1.33 – 3.47).
The researchers also observed that the median time to diagnosis was not significantly different across the different time periods (+4.5 days, 95% CI -20.5 days to +29.5) and the median time to treatment was actually shorter during the pandemic (-0.7 days, 95% CI -1.1 to -0.30).
The authors concluded that the COVID-19 pandemic led to substantial reduction in the detection of cancer in young adults but was also associated with an increase in cancer-related ICU admissions. They suggested that this was probably due to more severe baseline disease at diagnosis and that overall, their findings demonstrate a clear disruption to cancer diagnostic pathways in this age group which need to be addressed urgently in the recovery phase of the pandemic.
Citation
Saatci D et al. The impact of the COVID-19 pandemic on cancer diagnostic pathways in children, teenagers and young adults: a cohort study in England. NCRI conference 2021
4th October 2021
The research, which was conducted across multiple hospitals in Spain, compared data from the first year of the COVID-19 pandemic with data from the previous year. Of 1385 cases of CRC diagnosed over the two-year period, almost two thirds (868 cases, 62.7%) were diagnosed in the pre-pandemic year from 24,860 colonoscopies. By contrast, only 517 cases (37.3%) were diagnosed during the pandemic, which also saw a 27% drop in the number of colonoscopies performed, to 17,337
Those who were diagnosed with CRC between 15 March 2020 and 28 February 2021 were also older than in the pre-pandemic year, had more frequent symptoms, a greater number of complications and presented at a more advanced disease stage.
Experts say the fall is a consequence of the suspension of screening programmes and the postponement of non-urgent colonoscopy investigations during the pandemic. Fewer cancers were identified by CRC screening in the pandemic period, with just 22 (4.3%) cases found in comparison to 182 (21%) in the pre-pandemic year. During the pandemic, more patients were diagnosed through symptoms (81.2% of diagnoses) compared with the pre-pandemic year (69%).
Dr María José Domper Arnal, from the Service of Digestive Diseases, University Clinic Hospital and the Aragón Health Research Institute (IIS Aragón) in Zaragoza, Spain, and lead author of the study, commented “These are very worrying findings indeed – cases of colorectal cancer undoubtedly went undiagnosed during the pandemic. Not only were there fewer diagnoses, but those diagnosed tended to be at a later stage and suffering from more serious symptoms.”
There was a significant increase in the number of patients being diagnosed with serious complications – a sign of late-stage disease – with an increase in symptoms such as bowel perforation, abscesses, bowel obstruction and bleeding requiring hospital admission. These cases made up 10.6% pre-pandemic and 14.7% during the pandemic. The number of stage IV cancers being diagnosed rose during the pandemic year, with stage IV cases making up 19.9% of cases, in comparison to 15.9% in the previous year.
“Although these figures are across a population of 1.3 million in Spain, it’s highly likely that the same drop in diagnoses would have happened elsewhere across the globe where screening was stopped and surgeries postponed, especially in countries that were heavily impacted by COVID-19”, explained Dr Arnal.
“Colorectal cancer is often curable if it’s caught at an early stage. Our concern is that we’re losing the opportunity to diagnose patients at this early stage, and this will have a knock-on effect on patient outcomes and survival. We are likely to see this fall out for years to come.”
Source
Impact of the COVID-19 pandemic in the diagnosis and characteristics of colorectal cancer patients, presented at UEG Week Virtual 2021