This website is intended for healthcare professionals only.
Take a look at a selection of our recent media coverage:
17th July 2024
Diet and exercise interventions before and during pregnancy could lower cardiovascular risk in children, researchers have suggested.
Scientists at King’s College London (KCL) reviewed previous studies to examine the effectiveness of health interventions in obese women such as antenatal and postnatal exercise programmes and healthy diets for unborn children and the development of cardiovascular health.
Over half of women attending antenatal clinics in England and Wales are either obese or overweight, putting their unborn children at risk of heart issues in both childhood and later life.
The findings, published in the International Journal of Obesity, could help inform public health strategies and improve the heart health of future generations, the authors said.
The researchers reviewed existing data from sources such as PubMed, Embase, and previous reviews, to determine whether lifestyle interventions in pregnant women with obesity could reduce the chance of abnormal cardiac development in their offspring. In particular, they examined how the intervention could impact changes in the shape, size, structure and function of the heart, known as cardiac remodelling, and related cardiovascular parameters.
After screening over 3,000 articles, eight studies from five randomised controlled trials were included in the review. Diet and exercise interventions introduced during these trials included antenatal exercise (n = 2), diet and physical activity (n = 2), and preconception diet and physical activity (n = 1). The children in the studies were under two months old or between the ages of three and seven.
The researchers found that lifestyle interventions in obese women could benefit the heart health of children. Interventions led to lower rates of heart wall thickening, normal heart weight and a reduced risk of high heart rates.
In all the reviewed studies, reduced cardiac remodelling and reduced interventricular septal wall thickness were reported as a result of diet and exercise interventions. In some of the studies, the interventions in diet and exercise led to improved systolic and diastolic function and a reduced resting heart rate.
Dr Samuel Burden, research associate in the Department of Women and Children’s Health at KCL, said: ‘Maternal obesity is linked with markers of unhealthy heart development in children. We reviewed the existing literature on whether diet and exercise interventions in women with obesity either before or during pregnancy can reduce the impact of this and found evidence that these interventions indeed protect against the degree of unhealthy heart development in their children.’
The researchers suggested that longitudinal studies with larger sample sizes and in older children are required to confirm these observations and to determine whether these changes persist to adulthood.
Dr Burden added: ‘If these findings persist until adulthood, then these interventions could incur protection against the adverse cardiovascular outcomes experienced by adult offspring of women with obesity and inform public health strategies to improve the cardiovascular health of the next generation.’
Evidence from The Academy of Medical Sciences earlier this year highlighted that early years health, which starts in pre-conception and goes through pregnancy and the first five years of life, is often overlooked in current policy but is crucial for laying the foundations for lifelong mental and physical health.
A version of this article was originally published by our sister publication Nursing in Practice.
16th May 2024
A lack of physical activity in children as they grow into adulthood causes significant heart damage that could put them at an increased risk of myocardial infarction and stroke in later life, a new study has found.
Researchers found that increased sedentary time in adolescence increases heart mass, leading to long-term impacts on the heart’s structure and function.
The findings, published in the European Journal of Preventive Cardiology, show that encouraging even light physical activity in children can positively impact their future cardiac health and reduce the risk of premature heart damage.
The preliminary results of this study were presented at the European Society of Cardiology Congress in August 2023.
Increasing levels of physical activity are known to improve cardiometabolic and vascular health among young people. This has led to the recommendation that children under 18 undertake an average of 60 minutes of moderate-to-vigorous-intensity physical activity daily.
However, there is limited research showing how sedentary time and physical activity affect changes in heart structure and function over time in children.
To address this issue, researchers from the Universities of Exeter, Bristol and Eastern Finland analysed data from 1,682 children and young people who are part of the University of Bristol’s Children of the 90s cohort.
Activity levels were measured using accelerometer devices at ages 11, 15 and 24, including time spent sedentary or engaged in light-intensity physical activity or moderate-to-vigorous-intensity physical activity.
The researchers examined changes to their cardiac structural and functional properties during growth until young adulthood through echocardiography measurements at ages 17 and 24.
Blood samples were also measured for markers of cardiovascular risk including low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides, glucose, insulin, and high-sensitivity C-reactive protein. Blood pressure, heart rate, smoking status, socio-economic status, family history of cardiovascular disease, and dual-energy X-ray absorptiometry measured fat mass and lean mass were accounted for in the analyses.
At age 11, the children spent an average of six hours per day in sedentary activities, which increased to nine hours per day by young adulthood. The researchers found this significant increase in sedentary time contributed 40% of the total increase in heart mass seen in participants from ages 17 to 24.
The results were similar in children and adolescents with either normal weight or overweight and obesity, and in children with either normal blood pressure or high blood pressure.
However, the increase in cardiac mass was reduced on average by almost half (49%) over the seven-year observation period due to light physical activity. This involved participation in activities such as walking, cycling, playing in the playground and gardening for at least three hours per day, combined with decreasing sedentary time.
In comparison, for each additional minute of moderate-to-vigorous physical activity during childhood, the researchers found a 5% increase in cardiac mass out of the total expected increase occurring between adolescence and young adulthood.
They say their findings show that sedentary time contributes eight times more to increased cardiac mass than moderate-to-vigorous physical activity, the latter of which is associated with physiological increase.
The researchers suggest that childhood sedentariness causes increased body fat, inflammation, blood pressure, lipid levels, arterial stiffness and subsequent cardiac enlargement, which leads to poor cardiac health later in life.
Professor Andrew Agbaje, professor (associate) of clinical epidemiology and child health at the Institute of Public Health and Clinical Nutrition, School of Medicine, Faculty of Health Sciences, University of Eastern Finland, said: ‘Childhood sedentariness is a ticking time bomb, and tackling the problem should be a public health priority. Light physical activity is the only effective antidote against sedentariness and it’s fairly easy to accumulate three to four hours a day.’
Professor Agbaje added: ‘There should be a political will at local, national and global levels to promote light physical activity. We need to act now because the economic and health cost of sedentariness may become unbearable. Public health experts, health policymakers, paediatricians and parents should encourage kids to participate in daily light physical activity straight away.’
A version of this article was originally published by our sister publication Nursing in Practice.
12th February 2024
Regular bouts of moderate to vigorous physical activity can protect patients with type 2 diabetes from developing kidney disease, a new study has found.
Overweight and obese people with type 2 diabetes who undertook moderate to vigorous physical activity every week were significantly less likely to progress to chronic kidney disease than those who undertook minimal physical activity.
Increasing cumulative exercise by just over an hour a week is linked to a 33% reduction in risk of renal disease. The researchers showed that the increase in physical activity is just as effective whether the extra exercise is undertaken in short bursts of less than 10 minutes or for long periods of 10 minutes and over.
The findings, published in the British Journal of Sports Medicine, show that being physically active is one of the most effective ways to prevent kidney disease in people with type 2 diabetes and can even help patients unable or unwilling to engage in physical activity for over 10 minutes.
Diabetes accounts for 30-50% of chronic kidney disease cases globally, making it the leading cause of renal disease. Patients who have diabetes and chronic kidney disease have a 10-fold higher risk of death from any cause compared with those who have diabetes alone.
To determine whether there was an association between physical activity and chronic kidney disease risk in patients with type 2 diabetes, the researchers undertook a secondary analysis of an activity tracker study, which was part of the US Look AHEAD trial.
The study involved 1,746 participants, with an average age of 58.
The participants were monitored for moderate to vigorous levels of physical activity and the extent of chronic kidney disease at the start of the study and again at one, four and eight years later.
Chronic kidney disease was defined as a deterioration of at least 30% in the estimated glomerular filtration rate, the rate at which kidneys remove waste and extra water from the blood to make urine (less than 60 ml/min).
On average, participants undertook 329 minutes of moderate to vigorous physical activity every week. Over 80% of this was accumulated in periods of less than 10 minutes, with the remaining 12.5% in periods of more than 10 minutes.
Over the duration of the study, around one in three of the participants developed chronic kidney disease.
The participants who undertook the most moderate to vigorous physical activity, between 329 to 469 mins per week, were significantly less likely to progress to chronic kidney disease than those who did the least physical activity (under 220 mins).
The researchers found that for every 100 minutes of moderate to vigorous activity, there was a 9% lower risk of developing chronic kidney disease. This increased to 19% if the exercise sessions lasted for at least 10 minutes.
Participants who increased their weekly exercise tally by 63 minutes over the first four years of the study had a 33% lower risk of kidney disease than those with the most significant decrease of minutes per week. The improvement was seen whether the physical activity sessions were greater than or less than 10 minutes.
The researchers stated: ‘These findings are consistent with evidence that regular [physical activity] has direct anti-inflammatory effects, and can promote glycaemic control, improve insulin sensitivity, blood pressure, lipid profiles and other metabolic and cardiovascular risk factors, all of which are associated with renal function.’
The researchers suggest that all patients with diabetes should be encouraged to engage in as much exercise intensity as they can tolerate to maximise the benefits.
Just over an hour a day of walking, cycling, jogging or swimming could help overweight and obese adults with type 2 diabetes reduce their risk of progression to chronic kidney disease.
A previous study from 2022 showed that increased coffee consumption lowered rate of kidney function decline in people with type 2 diabetes.
A version of this article was originally published by our sister publication Nursing in Practice.
1st September 2023
With lack of time often cited as a barrier to undertaking physical activity, cramming a week‘s worth of exercise into a day or two may seem more achievable, especially if it provides comparable cardiovascular benefits to a more evenly distributed pattern. Hospital Healthcare Europe‘s clinical writer and resident pharmacist Rod Tucker considers the evidence.
It is abundantly clear that being physically active is associated with health benefits. Current guidance on physical activity for adults in most major countries in Europe is broadly similar: undertake either at least 150 minutes of moderate intensity activity a week or 75 minutes of vigorous intensity activity, plus two days a week of strengthening activities to work all of the main muscle groups.
Moreover, it is advocated that exercise is undertaken every day or spread evenly over four to five days a week.
But is there any evidence that achieving this amount of exercise is associated with health benefits? In a 2020 study, an international research group tried to answer this question.
The team looked at the association between attainment of the recommended amount of physical activity among a representative sample of US citizens, and all-cause and cause specific mortality.
Their analysis included 479,856 adults who were followed for a median of 8.75 years. The findings were very clear: undertaking the recommended amounts of physical activity reduced the risk of all-cause mortality by 40%. But not only that, such levels of activity lowered the risk of cardiovascular disease by 50% and the risk of cancer by 40%.
With clear evidence of the health benefits from undertaking the recommended levels of physical activity, surveys have also identified some notable and recognised barriers to exercising. One of the most consistently reported barriers is sufficient time to exercise, and this is seen irrespective of age and gender.
Although healthcare professionals may advocate that their patients engage in exercise as part of the health promotion message, it seems they don‘t always practise what they preach. In fact, research shows that lack of time is also a perceived barrier to exercise among doctors and nurses.
As well as insufficient time, a demanding workload gives rise to high levels of burnout and stress, and changing shift patterns can limit time and motivation, which all represent additional barriers to exercising among clinicians.
Evidence suggests that exercising for just one or two days a week could accrue the same health benefits seen among those who exercise more regularly throughout the week. For example, so-called ‘weekend warriors‘ – those who restrict physical activity to just one or two sessions per week – have a similar level of all-cause mortality compared to those who spread their physical activity over several days.
In fact, a 2023 meta-analysis of four studies with 426,428 participants found that the risk of both cardiovascular disease mortality and all-cause mortality in those compressing their activity into two days was 27% and 17% lower, respectively, when compared to those who were inactive.
However, a limitation of this analysis was that levels of physical activity were self-reported and therefore prone to misclassification bias.
With inherent self-reporting bias an issue, a recent study examined the value of accelerometer-derived data. Researchers recently set out to examine the association between a weekend warrior pattern of moderate-to-vigorous physical activity (MVPA) achieved over just one to two days, compared to the activity being spread more evenly, with the risk of incident cardiovascular events.
The researchers retrospectively analysed a UK Biobank cohort who provided a full week‘s worth of wrist-based accelerometer physical activity data. Individuals were classified into three groups: active weekend warriors, in which more than half of their total MVPA was undertaken over one to two days; regularly active, where exercising was spread throughout the week; and inactive, where less than 150 minutes of MVPA per week was undertaken.
They looked at associations between the different activity pattern and cardiovascular outcomes such as incident atrial fibrillation, myocardial infarction, heart failure and stroke. The findings were then adjusted for several potential covariates including age, sex, ethnicity race, alcohol and smoking and diet quality.
Data for 89,573 individuals with a mean of 62 years (56% female) were included in the analysis and who were followed for a median of 6.3 years. Interestingly, when stratified at the threshold of 150 minutes or more of MVPA per week, nearly half of the entire cohort (42.2%) were classed as weekend warriors.
The findings for atrial fibrillation, myocardial infarction, heart failure and stroke are summarised in the table below.
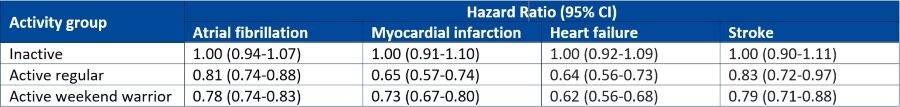
The accelerometer-derived study shows that engagement in physical activity, regardless of the pattern, is able to reduce the risk of a broad range of adverse cardiovascular outcomes. Therefore, although many healthcare professionals‘ working weeks may not permit specific exercising days, it seems that compressing physical activity into just two days per week, wherever possible, still achieves comparable health benefits.
So, whether it’s advice for patients or the foundation for personal fitness goals, the key message is to just keep moving.
31st August 2022
Greater regular physical activity reduces the risk of infection, hospitalisation, severe illness and death from COVID-19 in comparison to those who are inactive according to the findings of a systematic review and meta-analysis by a team of Spanish researchers.
Some degree of physical activity is better than none but greater regular physical activity is best for optimal health outcomes according to a World Health Organisation guideline from 2020. Physical activity has a beneficial impact on the immune system and also appears to have protective associations against infectious disease mortality.
Moreover, it also appears that the converse is true, particular in relation to COVID-19. For example, in a study of over 48,440 adult patients with a COVID-19, those who were physically inactive had a higher risk of hospitalisation, admission to intensive care and death compared to those who were consistently meeting physical activity guidelines.
But the extent to which greater regular physical activity impacts on adverse COVID-19 outcomes has not been quantified and was the purpose of the present systematic review and meta-analysis by the Spanish team.
The researchers looked for studies in adult patients with and without a COVID-19 diagnosis, where the exposure of interest was physical activity and when the outcomes of interest, e.g., infection, hospitalisation, were measured. The outcomes were assessed and pooled using odds ratios and relative risks.
Greater regular physical activity and COVID-19 outcomes
A total of 16 studies with 1,853610 participants and a mean age of 53.2 years (53% women) were included in the analysis. The amount of physical activity was self-reported in most of the studies though in cases where it was measured, this involved direct assessment using accelerometers or smart devices.
Adults engaging in greater regular physical activity and in comparison to those who were classed as inactive, had a lower risk of infection with COVID-19 (relative risk, RR = 0.89, 95% CI 0.84 – 0.95, p = 0.014), hospitalisation (RR = 0.64, 95% CI 0.54 – 0.76, p < 0.001), severe illness (RR = 0.66, 95% CI 0.58 – 0.77)) and death (RR = 0.57, 95% CI 0.46 – 0.71, p = 0.001).
In subgroup analysis, the researchers found that the beneficial effects of greater regular physical activity were independent of both study design and the instrument used.
The team also identified a non-linear dose-response relationship between physical activity when expressed as metabolic equivalent of task (MET)-min per week and severe COVID-19 illness and death but not for either infection or hospitalisation. In other words, there was a flattening of the dose response between regular physical activity and death at 500 MET-min per week and which is equivalent to 150 – 300 minutes of moderate intensity physical activity per week.
The authors concluded that their findings highlighted the importance of physical activity in lowering the risk of infection hospitalisation and severe outcomes in COVID-19, particularly where this level of activity matched the guideline-recommended amounts of 500-MET min/week.
Citation
Ezzatvar Y et al. Physical activity and risk of infection, severity and mortality of COVID-19: a systematic review and non-linear dose–response meta-analysis of data from 1 853 610 adults Br J Sports Med 2022
18th July 2022
‘Weekend warriors’ who restrict physical activity to just one or two sessions per week appear to have similar levels of all-cause and cause-specific mortality compared to those who are regularly active, i.e., spread their physical activity over several days. This was the conclusion of a large, prospective cohort study by an international group of researchers.
Physical activity guidelines for Americans (and which are broadly similar across the world) recommend that adults should do at least 150 to 300 minutes a week of moderate-intensity, or 75 to 150 minutes a week of vigorous-intensity aerobic physical activity. In addition, the guidelines advocate muscle strengthening activities of moderate or greater intensity on two days or more each week.
Furthermore, the evidence to date suggests that when adults engage in the recommended levels of physical activity, there is a greatly reduced risk of all-cause and cause specific mortality. Only a single study has examined the mortality benefits achieved by weekend warriors and suggested that it may be sufficient to reduce all-cause mortality risks, in comparison to those who are insufficiently active.
However, it is less clear whether concentrating the recommended amounts of physical exercise into one or two sessions (e.g., weekend warriors) provides the same mortality benefits as observed by those who are physically active throughout the week.
In the present analysis, researchers examined the all-cause and cause-specific mortality between weekend warriors and those who were regularly active using data from the US National Health Interview Survey from 1997 to 2013 and linked this information to a national death index.
They classified individuals as physically active (150 minutes of activity/week) or inactive (< 150 minutes/week). Among those deemed physically active, individuals were sub-divided into weekend warriors (1 – 2 sessions/week) or regularly active (> 3 sessions/week).
The main outcomes of interest were all-cause, cardiovascular and cancer-related mortality. In regression models, adjustments were made for several factors including age, gender, ethnicity and various lifestyle factors such as smoking status, alcohol intake and co-morbidities.
Weekend warriors and all-cause mortality
A total of 350978 individuals with a mean age of 41.1 years (50.8% women) were followed-up for a median of 10.4 years. More than half (52.5%) were deemed physically inactive, 3% weekend warriors and the remaining 44.5% regularly active. During the period of follow-up there were 21 898 deaths including 4130 from cardiovascular disease and 6034 from cancer.
When compared to those deemed physically inactive, the adjusted hazard ratio (HR) for all-cause mortality was 0.92 (95% CI, 0.83 – 1.02) for weekend warriors and 0.85 (95% CI 0.83 – 0.88) for regularly active participants. The HR for cardiovascular disease mortality were also similar for weekend warriors (HR = 0.87) and and those who were regularly active (HR = 0.77), as were the cancer-related HRs.
But when researchers compared mortality between weekend warriors and those who were regularly active, the all-cause, cardiovascular and cancer-related mortality hazard ratios, were also very similar, even after adjustment for the amount and intensity of physical activity undertaken.
The authors concluded that there were no significant differences for any cause mortality among those who were physically active, irrespective of whether the sessions were undertaken throughout the week or concentrated into one or two sessions.
Citation
dos Santos M et al. Association of the “Weekend Warrior” and Other Leisure-time Physical Activity Patterns With All-Cause and Cause-Specific Mortality: A Nationwide Cohort Study JAMA Intern Med 2022
17th June 2022
Patients with coronary heart disease (CHD) who continue to be physically active over time and even those who reduce their activity, have a significantly lower risk of all-cause mortality compared to those who remain physically inactive.
This was the key finding from a meta-analysis by a team of researchers from Switzerland and Colombia.
Cardiovascular diseases are the leading cause of mortality around the world with an estimated 17.9 million deaths in 2019 and which represented 32% of all global deaths. One modifiable risk factor for cardiovascular disease (CVD) is physical activity and in a 2017 study found that a higher level of recreational and non-recreational physical activity was associated with a lower risk of all-cause mortality and CVD events.
However, whilst there are clear benefits from increased levels of physical activity with respect to all-cause mortality among those with CHD, what is less clear, is the impact of changes in physical activity over time.
For the present study, the researchers performed a systematic review and meta-analysis to examine the association between longitudinal trajectories of physical activity and both all-cause mortality and cardiovascular disease mortality in those with CHD.
The team included studies with a longitudinal design in adults with CHD and which provided data on all-cause and CVD mortality.
For the purposes of the analysis, the researchers examined the changes in all-cause mortality by different levels of reported physical activity trajectories. For example, those who remained inactive, those who increased their physical activity and finally individuals who decreased their activity level over time.
For the analysis, hazard ratios were calculated and regression models were adjusted for age, gender, ethnicity, smoking status, alcohol intake and co-morbidities. All of the studies assessed physical activity using validated questionnaires.
All-cause mortality and physical activity trajectories
A total of 9 articles were included in the final analysis, all of which were prospective in nature with 33,576 patients with an overall mean age of 62.5 years and the proportion of women ranging from 18 to 56%.
Compared to those who remained inactive over time, the risk of all-cause mortality was 50% lower among those who remained active (hazard ratio, HR = 0.50, 95% CI 0.39 – 0.63), 45% lower for those who increased their level of activity (HR = 0.55, 95% CI 0.44 – 0.70).
Moreover, even among those who had been active but who became less active, there was still a 20% lower all-cause mortality risk (HR = 0.80, 95% CI 0.64 – 0.99).
These reductions in risk were similar for cardiovascular mortality. For example, it was 51% lower for those who remained active (vs inactive) however, it became non-significant for those whose activity levels had reduced over time (HR = 0.91, 95% CI 0.67 – 1.24).
The authors concluded that there was a possible protective mortality benefit of either increased or continued activity among patients with CHD and suggested that physical activity trajectories should be considered in clinical practice.
Citation
Gonzalez-Jaramillo N et al. Systematic Review of Physical Activity Trajectories and Mortality in Patients With Coronary Artery Disease J Am Col Cardiol 2022
21st April 2022
The risk of depression can be greatly reduced even by undertaking lower amounts of the recommended levels of physical activity according to the results of a meta-analysis by researchers from the MRC Epidemiology Unit, University of Cambridge School of Clinical Medicine, Cambridge, UK.
Depression is a common, global mental disorder that is believed to affect 5% of the population. Moreover, a 2015 meta-analysis estimated that every year, 14.3% of global deaths, approximately 8 million deaths, can be linked to mental disorders. With such a high prevalence and associated mortality, much needs to be done to try and prevent or reduce depression risk.
One possible mitigating factor is physical activity and according to one systematic review, promoting physical activity may serve as a valuable mental health promotion strategy in reducing the risk of developing depression. In fact, a 2018 meta-analysis of prospective cohort studies suggested that the available evidence supports the idea that physical activity can confer protection against the emergence of depression regardless of age and geographical region.
With a good deal of evidence indicating a protective effect from physical activity, what remains uncertain is the strength or shape of the association between physical activity and depression.
For the present analysis, the UK team looked for trials that included any dimension of physical activity at three or more exposure levels, with at least 3,000 participants and with a follow-up period of not less than 3 years. Levels of physical activity were measured as marginal metabolic equivalents task hours per week (mMet-h/wk), where 1 Met represented the resting metabolic rate and 8.8 mMet-h/week was equivalent to the recommended weekly amount of physical activity. The outcome of interest was depression, major depressive disorder and elevated depression symptoms.
Depression risk and physical activity levels
The literature review identified 15 eligible publications including 191,130 participants (64% women) contributing 28,806 incident depression events and 2,110,588 person-years.
The results suggested an inverse and curvilinear dose-response between physical activity and depression, such that relative to adults who did not report undertaking any physical activity, those doing at least half of the recommended activity (4.4 mMet-hrs/week), had an 18% lower risk of depression (relative risk, RR = 0.82, 95% CI 0.77 – 0.87).
Among those achieving the recommended amounts of activity (8.8 mMet-hrs/week), there was a 25% reduced risk of depression (RR = 0.75, 95% CI 0.68 – 0.82) and this reduction was the same for major depression and slightly lower for elevated depressive symptoms (RR = 0.73). However, interestingly, there was little apparent benefit derived from increasing activity to 17.5 mMet-hrs/week (RR = 0.72, 95% CI 0.64 – 0.81), for each of the three outcome measures.
Using potential impact fraction (PIF) analysis, the authors calculated that around 11.5% of incident depression could have been prevented in adults who achieved at least 8.8 mMet-hrs/week of physical activity.
Translating their findings into practical advice, the authors stated that accumulating an activity equivalent to 2.5 hours/week of brisk walking was associated with a 25% lower risk of depression and that achieving half of this level, reduced the risk by 18% compared with those who undertook no physical activity.
They concluded that substantial mental health benefits accrue from the achievement of physical activity levels even below those currently recommended.
Citation
Pearce M et al. Association Between Physical Activity and Risk of Depression: A Systematic Review and Meta-analysis JAMA Psychiatry 2022
28th March 2022
Increased physical activity levels in older adults with high serum levels of neurofilament light chain (NFL) leads to a reduction in the rate of cognitive decline. This was the conclusion of a study by researchers from the Rush Institute for Healthy Aging, Rush University Medical Center, Chicago, US.
Neurofilament light chain is a neuronal cytoplasmic protein expressed in large calibre myelinated axons. Furthermore, in both central nervous system and peripheral nervous system diseases associated with axonal injury or degeneration, the concentration of NFL has been found to increase in both cerebrospinal fluid (CSF) and blood.
In addition, levels of CSF NFL are associated with cognitive impairments in patients with Alzheimer disease and fronto-temporal dementia. As a result, it has been suggested that NFL could be used to predict the development of sporadic Alzheimer’s disease and cognitive decline. One factor which appears to be associated with a reduced cognitive decline is physical activity and in a 2011 meta-analysis, the authors concluded that there was a significant and consistent protection for all levels of physical activity against the occurrence of cognitive decline.
For the present study, the US team wanted to examine whether among individuals with high NFL concentrations, increased physical activity was associated with a slowed rate of cognitive decline over time. They turned to the Chicago Health and Aging Project (CHAP), which is a longitudinal population study of common chronic health problems of older persons and in particular, risk factors for incident Alzheimer’s disease.
Blood samples were taken and the concentration of NFL measured at baseline and during each follow-up appointment and dichotomised as low (< 25.5 pg./ml) or high (> 25 pg./ml). Levels of physical activity were self-reported divided into three groups: little activity, medium and high, in which the latter group reported physical activity levels > 150 minutes/week.
A number of cognitive tests were used to assess global cognitive function. The main outcome measure was the association of baseline activity and NFL concentrations with changes in global cognitive function over time.
Increased physical activity and NFL in relation to cognitive decline
A total of 1158 participants with a mean age of 77.4 years (63% female) were included in the study. The mean level of physical activity per week was 170.78 minutes and the geometric mean NFL concentration was 26.1 pg/ml.
Among those with a high NFL levels, indicating more axonal injury, individuals engaging in medium physical activity (< 150 minutes/week), had a 12% slower rate of global cognitive decline compared to those in the low physical activity group. Similarly, those with increased physical activity (i.e., the high group), had a 36% slower rate of decline in comparison to the low physical activity group.
Interestingly, the the rates of cognitive decline were also higher among those with lower levels of NFL, i.e., with less neural damage. For example, in comparison to the group who undertook little or no physical activity, those who undertook medium physical activity had a 43% slower decline and the high activity group, at 30% slower decline.
The authors concluded that among older adults with high levels of serum NFL, increased physical activity levels were associated with a slower rate of cognitive decline. They added that future studies should examine the relationship between cognitive decline and different forms of exercise such as aerobics and strength training.
Citation
Desai P et al. Examination of Neurofilament Light Chain Serum Concentrations, Physical Activity, and Cognitive Decline in Older Adults JAMA Netw Open 2022.
22nd February 2022
Undertaking physical activity for a minimum of 20 minutes every day is associated with a significant reduction in the risk of cardiovascular disease in elderly patients, according to the results of a longitudinal study by a team of researchers from the department of Cardio-thoraco-Vascular Sciences and Public Health, University of Padua, Italy.
There is already good evidence demonstrating that higher recreational and non-recreational physical activity is associated with a lower risk of mortality and CVD events. In addition, the risk of cardiovascular disease has been found to reduce in a linear manner with increasing levels of physical activity up to around 41%.
However, whilst there are clear health benefits derived from engaging in greater levels of physical activity, few of the reviewed studies focused on older (≥65 years) adults. Furthermore, there is little evidence on the association of activity trajectories and specific cardiovascular outcomes, though where this has been examined, the authors concluded that cardiovascular health trajectories may be associated with subsequent CVD risk.
With an increasingly ageing population, for the present study, the Italian team sought to explore the relationship between different trajectories of activity and cardiovascular events in older men and women. The team turned to the Progetto Veneto Anziani study which has followed over 3,000 Italians aged 65 years and older from 1995 and who had follow-up visits after 4 and 7 years.
Individuals underwent physical examinations and completed various medical questionnaires, assessing smoking status, alcohol use, co-morbidities etc and morbidity and mortality data collection was extended until 2018.
The levels of physical activity were collected at baseline and at follow-up appointments and individuals were subsequently categorised as active if they engaged in > 20 minutes of activity each day or inactive if < 20 minutes each day.
Based on information collected from participants, the researchers defined four separate exercise trajectories: stable-low (i.e., essentially inactive); high-decreasing (active – inactive); low-increasing (inactive-active) and finally stable-high (maintaining activity).
Outcomes of interest were a diagnosis of cardiovascular disease (CVD), coronary heart disease (CHD), heart failure (HF) and stroke.
Physical activity and cardiovascular outcomes
A total of 2754 individuals with a mean age of 75.1 years (60.2% female) were included and followed-up for a period of 20 years. During the 20-year follow-up, there were 1037 incident cardiovascular events.
The rates of incident coronary heart disease and heart failure were significantly associated with being active compared to inactive. For example, there was a lower risk of CVD (hazard ratio, HR = 0.74, 95% CI 0.58 – 0.94), CHD (HR = 0.66, 95% CI 0.50 – 0.87) and HF (HR = 0.72, 95% CI 0.53 – 0.98) in men but not for strokes. In contrast, none of these relationships were significant for women.
However, physical activity was associated with a significantly reduced risk of overall mortality in both men (HR = 0.72, 95% CI 0.62 – 0.84) and women (HR = 0.81, 95% CI 0.72 – 0.92).
Considering the dose-response relationship, the risk reduction for any incident cardiovascular event was associated with doing at least 20 minutes of activity each day for those aged 70.
Using trajectories of physical activity and using the stable-low category as the reference point, for any cardiovascular disease, the fully adjusted hazard ratio was 0.48 (95% CI 0.27 – 0.86) for men in the stable-high category, i.e., a 52% reduced risk of CVD in those who maintained high levels of activity in later life. Nevertheless, this association was not significant for women.
The authors concluded that greater amounts of physical activity in older adults was associated with a reduced risk of CHD and heart failure and that a minimum of 20 minutes each day of moderate to vigorous activity should be recommended for the greatest cardiovascular benefits.
Citation
Amidei CB et al. Association of physical activity trajectories with major cardiovascular diseases in elderly people Heart 2022