This website is intended for healthcare professionals only.
Take a look at a selection of our recent media coverage:
28th April 2023
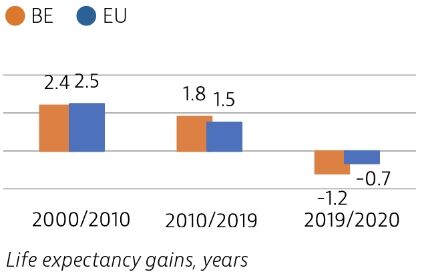
Life expectancy in Belgium remains slightly above the EU average, but it temporarily fell sharply in 2020 because of deaths due to Covid-19.
While the Belgian health system provides good access to high-quality care, the Covid-19 pandemic highlighted important challenges with prevention and public health, the health workforce and quality of care in long-term care facilities for older people. The pandemic stimulated many innovative practices in Belgium that could be expanded to build a more resilient healthcare system.
Life expectancy in Belgium increased more than the EU average between 2010 and 2019, but fell by more than a year in 2020 because of deaths due to Covid-19. About 60% of the Covid-19 deaths in 2020 were among residents in long-term care facilities. As in many other countries, the mental health of many young people and adults in Belgium deteriorated greatly during the pandemic, with reports of anxiety and depression reaching much higher levels than in previous years.
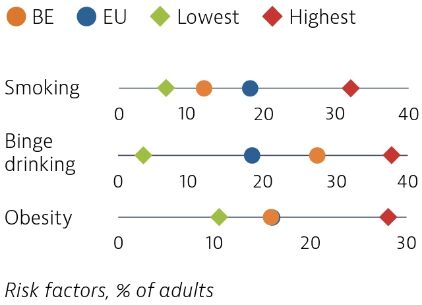
Risk factors for health are major drivers of ill health and mortality in Belgium. While tobacco consumption has substantially decreased over the past two decades, 15% of adults were daily smokers in 2018. Nearly 30% of adults reported regular heavy alcohol consumption in 2018, a rate well above the EU average. About 16% of adults were obese in 2018, close to the EU average, but up from 12% in 2001. Overweight and obesity among 15-year-old adolescents have also increased to 17% in 2018, up from 11% in 2002.
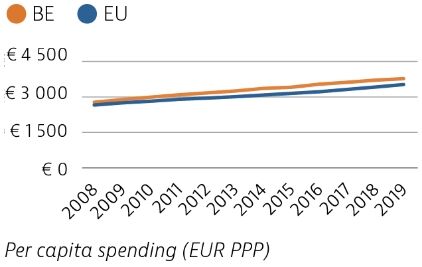
Health spending per capita increased slowly between 2008 and 2019 and remains higher than the EU average. In 2019, health spending accounted for 10.7% of GDP, up from 9.6% in 2008, and also a higher share than the current EU average (9.9%). Public spending accounted for 77% of overall health spending – slightly less than the EU average of 80%.
Avoidable mortality was slightly lower than the EU average before the pandemic, but higher than in many other western EU countries. This suggests that more could be done to save the lives of people through health promotion and a reduction of risk factors and through better healthcare.

Although access to healthcare in Belgium is generally good, the Covid-19 pandemic significantly affected access to care in 2020: 22% reported forgone care during the first 12 months of the pandemic, which is close to the EU average of 21%. Growing use of teleconsultations helped maintain access to care during the pandemic.

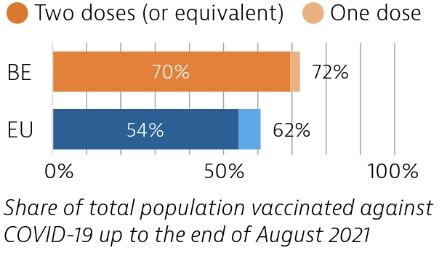
Belgium was among the EU countries hardest hit by the Covid-19 pandemic in numbers of cases and deaths relative to its population size, particularly during the first wave. Belgium accelerated its vaccination campaign in the first half of 2021. By the end of August 2021, 70% of the population had received two doses (or equivalent) of a Covid-19 vaccine.
OECD/European Observatory on Health Systems and Policies (2021), Belgium: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels.
13th April 2023
It’s been almost a year since the Cleveland Clinic London opened its doors at 33 Grosvenor Place, London.
The 184-bed private hospital, owned by the Cleveland Clinic, a US non-profit multispecialty academic medical centre founded in 1921, provides a suite of cardiology services for both common and complex heart conditions.
Among those is a comprehensive transcatheter aortic valve implantation (TAVI) programme, which treats aortic stenosis through a tiny groin incision, and minimal access endoscopic mitral valve surgery.

Professor Olaf Wendler, a consultant cardiac surgeon with more than 30 years’ experience and chair of the Heart, Vascular and Thoracic Institute at Cleveland Clinic London, shares the inspiration for his chosen career path and shines a light on the pioneering work being undertaken at the facility.
I did my surgical training at the Medical School Hannover and the Heart Center Leipzig in Germany and then became clinical lead at the University Saarland, Germany. I was the director of cardiovascular services at King’s College London from 2006 to 2012 when I was promoted to professor of cardiac surgery at King’s College London. In 2019, I was appointed chair of the Heart, Vascular and Thoracic Institute at Cleveland Clinic London.
I was particularly attracted by how easily patients can recover from major cardiac surgery if they get the right surgeon. Throughout my career, I have been heavily involved with developing new techniques and devices that reduce the trauma of surgery for patients. The focus of my surgical and academic works is in the field of heart valve surgery. Together with my cardiology colleagues, we have developed techniques to repair and preserve native heart valves, as well as minimally invasive and keyhole therapies to replace heart valves. In 2007, the teams and I performed the UK’s first transapical TAVI procedure, followed by numerous innovative therapies. My expertise also lies in complex and repeat combined heart procedures, complete arterial coronary bypass surgery and complex thoracic aortic surgery.
Cleveland Clinic London employs around 1,150 caregivers, including over 450 nurses. Almost 300 doctors work with us, with the majority doing all private work exclusively here and maintaining their NHS practices. The hospital is the newest location in Cleveland Clinic’s expanding global footprint and the second in London, following the opening of Cleveland Clinic Portland Place Outpatient Centre in September 2021. The Cleveland Clinic health system, which employs more than 77,000 caregivers worldwide, has pioneered many medical breakthroughs including coronary artery bypass surgery, the first face transplant in the United States and, most recently, the first uterus transplant in the United States.
We have implemented the most comprehensive transcatheter heart valve programme in a London private hospital. Between June 2022 and February 2023, we performed 64 TAVI procedures under the leadership of Professor Bernard Prendergast and Professor Simon Redwood. Most of our aortic valve and mitral valve surgery is performed through minimally invasive procedures to allow the faster recovery of patients. We also preserve native heart valves and repair them whenever possible – not only the mitral valve but also the aortic valve.
Treatment for narrowed and leaking heart valves in the most challenging patients is also a focus. Consultant cardiologist Professor Baumbach performed the first valve implantation into a leaking aortic valve in a London private hospital. The above service is supported through world-class cardiovascular imaging services with imagers part of the multidisciplinary teams.
Our surgical and interventional outcomes have been excellent with no in-hospital mortalities after cardiac surgery and intervention since opening. We also have regular M&M meetings to detect not only mortality but also morbidity after surgery and intervention.
Our thoracic surgeons have successfully started to perform robotic thoracic surgery to reduce the side effects in patients. It enables them to perform operations on the lung through keyholes, which shortens the recovery times of patients.
Robotic percutaneous intervention to treat patients with coronary artery disease is used to reduce procedure times for patients and as a result reduce radiation for patients and their treating physicians. It is a very new field. We plan to invest in a robot for this area and fund a research fellow through the Cleveland Clinic London charity to develop this further.
Professor Rinaldi, the most experienced cardiologist in the field of laser lead extraction in the UK, is our lead for electrophysiology. Laser lead extraction enables cardiologists to explant pacing leads, which connect pacemakers to the heart when they are broken or get infected. It is more frequently needed in patients who have been treated with heart pacemakers or defibrillator devices. It is a technology that currently isn’t available in private UK facilities – we are investing in it.
We are also investing in laser coronary angioplasty, a technique used to open up the most challenging obstructions in patients with coronary artery disease and isn’t currently used in private UK facilities.
Research has found evidence that high-intensity exercise can acutely increase the risk of sudden cardiac arrest in individuals with underlying cardiac disease. This can also increase the risk of heart rhythm disorders, especially for the minority with hypertrophic cardiomyopathy or coronary heart disease.
We work with Professor Sanjay Sharma, who pioneered this emerging field of cardiac care and works as a cardiologist for the English Institute of Sport, British Rugby League and the British Lawn Tennis Association.
He has in-depth experience in heart muscle diseases, heart valve diseases, arrhythmias and sudden cardiac death prevention.
Our team can screen, assess, and care for any condition. We treat:
Our team of expert consultants includes Professor Aldo Rinaldi, Professor Pier Lambiase, Dr Magdi Saba, Dr Simon Sporton, Dr Sabine Ernst, Dr Tom Wong, Dr Manav Sohal and Dr Niraj Varma. They are supported by leading cardiac physiologists and nurses. Sophisticated interventions including ventricular ablation, where the heart is approached through keyholes from outside and inside are performed. The team also has expertise in implantable devices that can re-synchronise the heart and improve symptoms in patients with chronic heart failure.
We facilitate regular meetings for postgraduate training. The next is planned to take place in October 2023 at the Royal Society of Medicine with a focus on cardiovascular medicine. We also facilitate virtual meetings for GPs and physicians.
Our cardiac academics have a particular focus on the treatment of coronary artery disease and minimally invasive heart valve therapy. In addition, we also have a very strong team for the treatment of aortic disease, with treatment capabilities from the heart to the legs. Our academic cardiologists have an international reputation for the transcatheter keyhole replacement and repair of heart valves.
We have a clinical trials unit led by Professor Charles Knowles and just recently approved our first cardiology trial, which focuses on the keyhole implantation of a heart valve prosthesis into the tricuspid valve. This trial is led by Dr Sam Dawkins but is in the very early stages.
The Fame 3 study on the treatment of coronary heart disease. Patients with three-vessel coronary artery disease have been found to have better outcomes with coronary artery bypass grafting (CABG) than with percutaneous coronary intervention (PCI). However, studies in which PCI is guided by measurement of fractional flow reserve (FFR) have been lacking.
This study, published last year, showed that in patients with three-vessel coronary artery disease, FFR-guided PCI was not found to be non-inferior to CABG with respect to the incidence of a composite of death, myocardial infarction, stroke or repeat revascularisation at one year.
Professor Prendergast and I have co-authored European guidelines for valvular heart disease, valve endocarditis and coronary artery disease.
Healthcare costs are steadily increasing at a time when the NHS is facing significant challenges. With waiting lists for diagnostics and procedures steadily growing, it is critical that private organisations develop the clinical governance frameworks needed to provide guideline-driven, safe and effective medical care.
Explore the latest advances in clinical care, delivered by renowned experts from recognised Centres of Excellence, at the HHE Clinical Excellence in Cardiovascular Care event on 10 May 2023. Find out more and register for free here.

Vince Walker has worked at the Royal Stoke Hospital for 14 years and is currently head of cardiac arrhythmia diagnostics and electrophysiology.
Training as a cardiac physiologist in 2009, Vince Walker has a particular interest in technology in heart care and has since completed a postgraduate accreditation with the British Heart Rhythm Society (BHRS) and the International Board of Heart Rhythm Examiners (IBHRE) for both cardiac devices and cardiac electrophysiology.
Walker is passionate about using technology within the NHS to help manage patients with detectable conditions, such as atrial fibrillation (AF), to deliver “cost-effective, accurate and swift diagnostics to patients”.
He shares how he helped evolve the stroke care pathway at his hospital and why tech and diagnostics are the future of healthcare.
The link between AF and stroke is established but not fully understood. The immediate and long-term effects of a stroke on an individual, their family and the NHS is significant. It is fiscally costly to treat and manage a patient following an embolic stroke and, more importantly, the personal cost to an individual patient is often devastating. However, there is a general acceptance that AF-related stroke is largely preventable with prolonged cardiac monitoring to detect AF and anticoagulation therapy.
I worked closely with Dr Indira Natarajan and Rachel Powell in neurology stroke services to develop a pathway for post-TIA/stroke patients to access implantable cardiac monitors as an option to help to detect AF after cryptogenic stroke. In the wider stroke population, conventional arrhythmia diagnostics using ambulatory monitoring fails to reveal a high incidence of AF and cannot rule out paroxysmal AF as a risk factor for stroke. This equates to approximately 25% of referrals into the arrhythmia monitoring service.
A small pilot study at the Royal Stoke Hospital comparing 50 post-stroke patients inserted with the device to a post-stroke cohort fitted with conventionally ambulatory monitors (observed retrospectively over six months) was found to have considerably different diagnostic yields to detect AF (15% vs <1%). This led to the development of our direct access service and the use of these insertable heart monitors in the most appropriate post-stroke patients.
It led to expedited diagnosis of AF and intervention with anticoagulation compared to traditional follow-up methods. Waiting times are often shorter for device implantation compared to ambulatory monitoring.
The pathway extends to patients that have made a good recovery post-stroke and would be considered for anticoagulation if AF was detected. There is also the additional therapeutic value in patients diagnosed with AF; it may be the case that symptoms related to the rate of arrhythmia occur as events become more frequent. We are currently observing patients with detected AF and their long-term outcomes following treatment with respect to drug therapy, ablation or even pacemaker therapy.
Post-stroke patients would be referred for 24-hour ambulatory or Holter cardiac monitoring. This would be performed approximately six weeks later in an outpatient clinic. The results of the monitors would generally be reported back to the stroke team within seven days. If AF was not detected it would be typical to offer longer-term monitoring of up to seven days, but this would often require a further waiting time of six weeks or longer. Essentially, referrals for prolonged cardiac monitoring may typically require several months of waiting and still be very unlikely to diagnose AF.
The cost savings are difficult to appreciate through secondary care budgets. The stroke physicians believe the biggest cost saving is through the reduction of AF-related stroke by means of anticoagulation, better patient outcomes and lesser stroke severity, which, if reduced, may show more of a cost saving in the social care sectors. In a related study, the approach led to a 64% reduction in risk of stroke and a 25% reduction in mortality. Regrettably, this pathway is geared toward patients who have already transited secondary care treatment for which the initial cost has already been incurred. The evidence for device-detected AF, anticoagulation and relative stroke risk reduction is currently unclear, but, by developing pathways, we hope trends will emerge to further these pathways in the future.
I spent two years [2015-2017] working to consolidate the more technical aspects of cardiac devices and to really understand the potential and limitations of device care with patients. I now lead a large cardiac rhythm management (CRM) diagnostics service at University Hospitals of North Midlands NHS Trust (UHNM) that delivers approximately 1,200 conventional ambulatory ECG monitors and 50 insertable devices per month through a team of 15 specialist arrhythmia physiologists and clinical scientists.
Typically, I work an 8am to 5pm day with a one-in-seven on-call out-of-hours and overnight. I hold a clinical role within cardiac devices and electrophysiology covering outpatient clinics and procedures undertaken in the cardiac catheterisation lab. In addition, I am the service lead for electrophysiology and cardiac rhythm management and lead a large team to deliver a nationally recognised service. I would not be in this position without such a motivated, enthusiastic and hardworking team aligned to the same goal.
Roles range from Band 2 technicians with a primary focus on the delivery of ambulatory monitors and 12-lead ECG in outpatient settings and on the front line in A&E to coordinate flow through other outpatient clinics such as echocardiography. Band 3 and 4 staff complete a similar role but with more responsibility and independence, often working out in the community where specialist support is not readily available.
Then Band 5 cardiac physiologists provide the majority of the more complicated tests, such as exercise tolerance tests, and are involved in cardiac catheterisation labs and the reporting of ECG data. Band 6 roles take on further responsibility within arrhythmia monitoring and are considered entry-level positions in postgraduate training opportunities within echocardiography or cardiac devices.
Finally, Band 7 members of staff are qualified within those advanced practice roles to provide the more complex tests and reports to diagnose or contribute to the diagnosis of cardiac conditions.
On a weekly basis, UHNM NHS Trust’s cardiac diagnostics department provides more than 500 echocardiograms, over 300 ambulatory monitors, more than 300 ECGs, 500 insertable transmissions and in excess of 500 pacemaker/defibrillator appointments.
The wider team comprises nearly 70 staff delivering 2,000 patient interactions per week. Organising this many investigations is challenging given the flexibility of the NHS, the time sensitivity required for certain inpatient tests and the reactive nature of the environment due to emergencies or higher priority activity with no notice.
Within the cardiac physiology and healthcare science team at UHNM, preceptorship is offered to newly qualified Band 5 staff to help consolidate knowledge, to motivate and inspire, and to provide exposure to staff into the three advanced areas of practice: echocardiography, device management and cardiac arrhythmia management.
Yes – with respect to the pathway and outcomes of MRI in patients with non-conditional cardiac devices. These are patients fitted with either pacemakers or defibrillators, who are considered unsafe to undergo MRIs. By following a risk-stratified MDT approach with cardiology, radiologists and physicists are actually safe to continue to MRI. Having a structured pathway may enable legacy device patients or those currently contraindicated to safely undergo MRI in certain conditions. We have submitted this strategy to publication and international conferences.
Another publication awaiting peer review is an observational piece that considers the safety and efficacy outcomes following MDT for cardiac device patients undergoing radiotherapy for the treatment of cancer.
We are also currently looking into why patients decline implantable cardioverter defibrillator (ICD) devices. We are also exploring a ‘One Hospital Care’ solution to help collect information to easily identify trends within services and pathways to improve current service provision or what we may need to alter and steer towards in the future.
I feel the largest changes in the area of cardiac arrhythmia management will be more related to the management of large amounts of data produced routinely by patients 24 hours a day, seven days a week.
Explore the latest advances in clinical care, delivered by renowned experts from recognised Centres of Excellence, at the HHE Clinical Excellence in Cardiovascular Care event on 10 May 2023. Find out more and register for free here.
It’s been 12 months since Sian Harding hung up her lab coat.
The emeritus professor of cardiac pharmacology, who led the cardiovascular division of the National Heart and Lung Institute (NHLI) at Imperial College London and the British Heart Foundation Centre for Cardiac Regeneration, retired last April following an illustrious career spanning more than 40 years.
To mark this first anniversary, Hospital Healthcare Europe caught up with the cardiac scientist to reflect on her career, the hurdles she overcame as a young graduate in a profession largely dominated by men and her top tips for female scientists hoping to follow in her footsteps.
I remember being at primary school and one of the dinner ladies asked what I wanted to do for a living. “Cut up dead bodies,” was my reply as I was being mischievous. I knew I wanted to do something with biology, but I didn’t want to be a doctor. I used to read encyclopaedias when I was eight or nine.
No, both my parents were artists. My mother went to Saint Martin’s School of Art in London and studied fashion. She met my father who was at the Guildford School of Art, and he later became a photographer. He had an element of scientific thinking in terms of focusing and lenses and would talk to me about that. I was desperate for a chemistry set, which he bought for me, along with a microscope and a telescope. He indulged all my whims.
When I was younger, it was not quite so normal for women to go into science. When I applied to Oxbridge there was only one place out of five for women; the rest were earmarked for men. Similarly, I got married at 18 and the college I applied to did not take married women. I thought I would not tell them and would apply and try and get in. I passed the exam but did not get a place, however I was very happy to go to King’s so it was not too much of a problem.
I’m quite capable of defending myself, and I’m not easily bullied, but it was mostly being ignored and underestimated at every turn. It wasn’t until later in my career – probably in my fifties – that I was in positions of authority.
As well as her work at Imperial and the British Heart Foundation, Professor Harding has held roles including past president of the European Section of the International Society for Heart Research, special advisor to the House of Commons Science and Technology Select Committee on Regenerative Medicine, fellow of the AHA, ESC and ISHR, and she was also on the board of the British Society for Gene and Cell Therapy. Professor Harding was also named scientific PI for the UK’s first clinical trial on myocardial gene therapy.
Perhaps the insight that came to me like a eureka moment in 2013 – that beta blockers were not just blockers but also involved in activating protective pathways.
Also, learning how to make cardiomyocytes from human skin samples. One of the problems with cardiomyocytes [cells responsible for the contraction of the heart] is that when they are outside of the adult heart, they lose that stimulation and start to atrophy and decay. You can only keep them for a couple of days in petri dishes to study them.
Now, we can make human cardiac cells – genetically matched to the donor – by taking a tiny biopsy of skin and converting that to stem cells. They can then be induced to develop into beating cardiomyocytes by growth factors that would be present in the early embryo.
In the lab we would make billions of these cells, which can form contracting sheets of engineered heart tissue, that would beat away in the dish for a year. We even had birthday parties for them!
Potentially, they could be transplanted back into the donor. There are a couple of very early trials of this now, so that has been amazing. These can also be used as a model system to show faulty genes and have the same abnormalities in beating as a patient’s own heart. Drugs could then be tested on these cells in the petri dish.
Men are extremely happy to have a lab full of women who are great workers and very cooperative, but there is always a point when those women try to become independent. It can be difficult for women in the lab to establish their work and be recognised for what they have done, not just an appendage of their previous mentor or boss.
We try to reduce institutional barriers to that. Still, the habits, especially of older males, to think of people like themselves when they’re considering who to promote or who to get onto a committee or who is going to get a grant is very ingrained. If you don’t keep pushing at it, they’ll just relapse and choose of the first person they can think of – often a man.
Pay attention not only to science but also to your career. Make sure you’re asking about the fellowships and pushing for the next stage when trying to get on the academic ladder or working in biotech.
Turn up to corporate events and things like evening receptions when someone is leaving. Just be around. When my daughter went to college, we moved closer to my work and I started doing more things. If people have seen you and understand you, they are more likely to think of you when they need someone.
Get onto committees – the way to do that is by being interested in the institution you are in. Understand your institution’s goals and nuts and bolts and match your behaviours to those.
Start on a small committee. If you show the right behaviour – that you can work in that environment, that you’re reliable and you understand what you’re supposed to be doing – then you’ll get on other bigger committees and important people will think you’re important because you’re on the same committee as them. They will have seen you operating. You don’t have to be a genius; you just have to do things properly, and then you’ll get into that world and work your way up.
Also, be around and informed. If you can introduce your institution or department to a person they could recruit, or a potential source of income, you will gain the attention of the committee or people in the higher echelons for being an interesting and useful person to know.
I’m still too big, really. I always have been, unfortunately. I do 30 minutes of exercise at least five days a week. I’ve got an exercise bike and I lift weights – resistance, rather than pumping iron – do intermittent fasting and try to look after my gut health by eating fermented foods.
A few years ago, my cholesterol was creeping up and I took statins as soon as I could. I was told I didn’t need to go on them, but I think statins are good drugs – much more effective at lowering cholesterol than any lifestyle intervention you can do. Plus, they have other effects on blood vessel health over and above the cholesterol. I had pre-eclampsia when I was pregnant, so I have been on blood pressure tablets all my adult life.
For any given day I’ve got Plan A, Plan B and Plan C. I don’t always tell my husband how finely planned everything is to avoid alarming him.
I published my book, The Exquisite Machine: The New Science of the Heart in September 2022. As a scientist, you must write in a very specific controlled way, you can’t use vivid language, and I wanted to learn how to write differently. I started it the year before Covid arrived, though publishing became slow during the pandemic with bookshops closed.
I’ve also gone back to my roots. As mentioned, my parents were artists, so I’ve been messing about taking several art courses on colour composition and painting. I thought I’d choose the easy one first – acrylic paint. It’s been very enjoyable. I was inspired by the Grayson Perry Art Club. You don’t have to be good at art to do it!
Explore the latest advances in clinical care, delivered by renowned experts from recognised Centres of Excellence, at the HHE Clinical Excellence in Cardiovascular Care event on 10 May 2023. Find out more and register for free here.

Dr Hannah Douglas is a consultant cardiologist specialising in adult congenital heart disease at Guy’s & St Thomas’ NHS Foundation Trust. She is also the lead cardiologist for heart disease in pregnancy, works on the pulmonary hypertension team and runs a private practice at London Bridge Hospital HCA Healthcare.
Dr Douglas tells Hospital Healthcare Europe why heart disease in pregnancy is on the rise, the impact this has on services and what needs to be done to manage it.
17 years. I graduated in 2006 and obtained my primary medical degree from Queen’s University Belfast. Most of my medical training was at the Royal Victoria Hospital in the city. I then went to work at St Thomas’ Hospital in London as a subspecialty fellow in congenital heart disease. My additional skills include transthoracic and transoesophageal echocardiography, which help clarify complex diagnoses and support procedures such as cardiac surgery and catheter lab interventions.
During my placements as a junior doctor, I was torn between both cardiology and obstetrics and gynaecology. I had some really challenging experiences with difficult high-risk patients during both rotations, but I enjoyed the nature of the work and the patient cohorts. I’ll never forget the pregnant lady who suffered a cardiac arrest due to an undiagnosed, underlying heart condition. It was a completely formative experience in my training as a junior doctor and, without a doubt, influenced my career choices. I realised that I could marry the two specialties by training towards congenital heart disease, which has always been the traditional pathway to access obstetric cardiology or heart disease in pregnancy care.
Heart disease is the leading cause of maternal death in the UK. There remains a healthcare gender gap between men and women, which becomes extremely visible in cardiovascular disease within female-centred fields such as antenatal and obstetric care. I see a significant proportion of the population with undiagnosed conditions, such as cardiomyopathies or heart muscle disorders, which may be asymptomatic but then destabilise due to the added cardiac demands of pregnancy.
The number of women who are of advanced maternal age coming through antenatal care is rising, which means we see an increase in the risk of complications such as high blood pressure, pre-eclampsia and cardiac events during pregnancy.
Acquired heart disease – which traditionally affected older people – also seems to be increasingly present in younger and younger members of the population due to social, demographic and lifestyle issues that increase cardiovascular disease risk factors.
Preventative medicine is not necessarily considered top of the priority list, so there are issues with resources, and there are huge healthcare cost implications, too. We can see multidisciplinary teams of up to 25 to 30 healthcare professionals managing a single woman with a high-risk cardiovascular condition so that we can deliver her and her baby safely in the correct environment.
Busy! Guy’s and St Thomas’ is a tertiary centre university teaching hospital in central London. I’m part of a large cardiovascular department comprising cardiologists and cardiac surgeons. We are a Level 1 adult congenital heart disease cardiac surgical centre and have a pregnancy heart team.
Across my week I am involved in acute inpatient cardiology work, outpatient clinics which comprise general cardiology, adult congenital heart disease and antenatal cardiology, theatre and catheterisation lab support, and frequent strategy, policies, planning and education meetings.
Within the fields of adult congenital heart disease and heart disease in pregnancy, I am what is described as an imaging cardiologist. I perform ultrasound-based imaging diagnostic tests to guide decision-making, monitor longer-term consequences of previous cardiac surgery, look at disease progression and support procedural interventions, such as keyhole type or trans-catheter procedures in the cath lab, but also in open heart surgery. Here, I help to evaluate before and after an operation as to what needs to be done and the repair work that has been done, working closely with my colleague cardiac surgeons.
At my practice in London Bridge Hospital, I look after patients with a range of general cardiac conditions, but I also see patients for pre-pregnancy risk assessment and counselling in women of childbearing age who may require optimisation of cardiovascular health before embarking on pregnancy.
Within the field of adult congenital heart disease, some of the most innovative procedures performed are trans-catheter redirection of complex holes in the heart. This gives our patients additional options other than open-heart bypass surgery.
My main research areas are related to cardiomyopathy in pregnancy and placental dysfunction, focusing on long-term cardiovascular outcomes in women with cardiovascular disease. I was part of a team that jointly published a paper on the prevalence of pre‐eclampsia and adverse pregnancy outcomes in women with pre‐existing cardiomyopathy.
It was a large, multi‐centre retrospective cohort study that found a modest increase in pre-term pre-eclampsia and a significant increase in foetal growth restriction (FGR) with pre-existing cardiac dysfunction. It found that the mechanism underpinning the relationship between cardiac dysfunction and FGR merited further research but could be influenced by concomitant beta blocker use.
Another paper I’m working on, which hasn’t been published yet, is the new British Society of Echocardiography Guidelines for the Pregnant Patient, which will be adopted as UK guidance for cardiac ultrasound scanning pregnant women with heart conditions.
Yes, we have constant fellowship posts across a range of sub-specialties within cardiology to include adult congenital heart disease.
Most of our fellows come from other parts of Europe and Asia where we build links with large international institutions to develop our own skills. We also provide additional experience to doctors towards the end of their training who require extra expertise or are planning to develop services similar to ours in other places.
There is an active research department within cardiology, and, in addition to this, we are at the forefront leading in complex surgical and trans-catheter interventions on patients of all ages and all types of congenital and acquired heart disease backgrounds.
Patient volume will continue to challenge us. We are growing in all areas of cardiology and specifically within the heart disease in pregnancy service. The number of patients we see face to face in the clinic and look after for antenatal surveillance is expanding all the time.
We also have a hub-and-spoke type sector-wide system whereby we reach out to train and support our colleagues in peripheral hospitals so that care can be delivered to women of perceived lower risk closer to home.
Challenges will continue within education and training, which needs to be constant and run rotationally, as well as staff turnover. We must educate medics, nursing staff, physiologists, midwives, interventionalists and anaesthetists – the list is endless. They need to be empowered to challenge their own learning and to recognise subtle or early risk factor signs. These might have important implications in minimising risks for women with a heart condition or who may develop a heart condition during pregnancy.
It is the responsibility of anyone who looks after women of childbearing age from menarche to menopause to address risk factors, contraception and family planning.
We also sometimes struggle to engage patients with this process – optimising women’s health before pregnancy is our long-term goal. Patients are getting older and sicker.
In pregnancy, we see increased advanced maternal age all the time. This is a complex caseload of patients, which will only continue to increase, and, therefore, the risks will increase with the patients.
It is, however, our privilege to provide such a service, and we never back down from a challenge!
Explore the latest advances in clinical care, delivered by renowned experts from recognised Centres of Excellence, at the HHE Clinical Excellence in Cardiovascular Care event on 10 May 2023. Find out more and register for free here.
Michael Henein is a professor of cardiology at Umeå University and Heart Centre, Sweden.

A consultant cardiologist in both Sweden and the UK, Michael Henein provides clinical cardiology services as well as transthoracic, stress and transoesophageal echo and carotid scanning at the Harley Street Clinic. He previously spent 15 years at the Royal Brompton Hospital as a consultant in cardiology and echocardiography having led the echocardiography department between 2001 and 2006.
To date, Professor Henein has supervised 21 PhD students at Imperial College and Umeå University and 100 MSc students between Imperial and Canterbury Christchurch University. He has also published more than 400 cardiology papers in peer-reviewed journals and edited seven textbooks.
Professor Henein is passionate about supervising international students and establishing strong academic partnerships with universities across the world. Here, he speaks to Hospital Healthcare Europe about the current projects he’s involved in.
Most of my projects are done with either my current or previous PhD students who’ve graduated. Personally, I think it’s very important to establish strong academic partnerships with international universities to help with the collaborative exchange of ideas, skills and approaches towards difficult clinical issues and research with good clinical and academic outcomes.
I’ve mostly worked with students from the UK, Sweden, Kosovo, Greece, Italy, Nigeria, Ireland, Egypt and China, all of whom have graduated and now hold important clinical and academic positions in their home countries.
Strong evidence suggests that people who undergo frequent strenuous exercise could develop arrhythmia or heart failure. We do not have any means by which we can predict which individuals will switch from being healthy to developing problems in the future, but we know it can end in disaster.
About six years ago, we looked at the effect of regular strenuous exercise on adolescents’ heart function. I’ve suggested to Flavio D’Ascenzi, one of my former PhD students, who is currently associate professor in Siena, in Italy, that we should get that group back on a 10-year follow-up. We would test them using the same methods used before to see who remains healthy and who may have developed changes and repeat again in another 10 years. These longitude studies are very difficult to design and ascertain, but this is a very good start with quite a unique group of individuals.
Hypertension is the most common disease we see in our cardiology practice. Long-standing high blood pressure is known to affect heart structure and function. Although it can be controlled, many people develop coronary heart disease (CHD) and strokes as a result. They could be symptomatic or asymptomatic, but it needs to be properly assessed.
We’re currently looking at identifying the predictors of CHD in these patients using non-invasive investigations like dobutamine stress echocardiography. This is a well-established, non-invasive investigation for significant coronary artery disease, which has zero radiation and is very patient friendly. Now’s the time to pull all the available evidence and do a detailed meta-analysis.
It’s very difficult to believe that atherosclerosis pathology chooses one branch of the aorta and doesn’t touch the rest. The scientific question here is, ‘is there any strong evidence to show that atherosclerosis disease is shared between different arterial systems?’.
In 2021, we published a paper on the results of a meta-analysis that compared the relationship between the phenotypic manifestation of coronary and carotid atherosclerosis – the two most commonly affected systems by atherosclerosis – using available imaging techniques. A total of 89 papers with 22,683 patients comparing carotid and coronary atherosclerosis were included in the analysis.
Our findings showed moderate relationship between carotid intima-media thickness and severity of coronary artery disease. Stenosis is important and not only serves in predicting the presence of severe disease but also helps in identifying patients demonstrating established arterial disease who need optimum risk factors control and follow-up management.
The results of the study supported the concept that atherosclerosis affects both carotid and coronary systems – although not always in an identical phenotypic manner. They also highlighted the benefits of examining carotid arteries whenever coronary artery disease is suspected.
The study was conducted on 63 patients presenting with unstable angina or positive stress test for myocardial ischaemia. All patients had CT scans of the carotid and coronary arteries using the conventional protocol and Agatston scoring system. Risk factors for atherosclerosis were also analysed for correlation with the extent of arterial calcification. In patients with coronary disease, the carotid calcification pattern appeared to be similar between the right and left systems in contrast to that of the coronary arteries. The coronary artery calcium (CAC) score correlated only modestly with the carotid score, despite being significantly higher at 10-fold. Hypertension was related to the CAC score, while diabetes and dyslipidaemia correlated with coronary calcification.
We can learn from one other. I have an interest in echocardiography, for example, but I cannot do it on my own. In Sweden Norrlands Heart Center, I had a technician who worked closely with me all the time. He updated me on new technology and the latest publications and software providers. We worked as a team and were able to look at our current practice and think, ‘why don’t we try this or that ourselves’. Myocardial deformation measurements using speckle tracking technology is an example that we developed recently. Over the years, I learned new things from this technician, who has since become a professor, and we have written many papers together.
It was at a heart centre in Germany in 2001/2002, many years before CT coronary scanning came to England. Back in those days, it was harder to convince anyone to start thinking about implementing them in routine practice. Now, this scanning for coronary disease is everywhere, which is wonderful, and time has changed, which is encouraging.
If we can open our eyes to what’s happening around us in Europe and North America and see the new procedures and techniques being developed locally, and have an open-minded approach, we can – in a humble way – be ahead of the game.
We can also be prepared for patients who are increasingly doing their own research on the internet and may catch us unaware when they come to us with questions about procedures or treatments they’ve found in operation in other countries.
Michael Henein is an advisory board member for HHE Clinical Excellence in Cardiovascular Care. He will be chairing a session entitled ‘Cardiology over 100 years’ at the event on 10 May 2023. Find out more and register for free here.

Amitava Banerjee is professor of clinical data science at the Institute of Health Informatics (IHI), University College London. He is also honorary consultant cardiologist at University College London Hospitals and Barts Health NHS Trust.
Whereas his research once primarily focused on big data in healthcare, Professor Banerjee says it is now almost 100% based on nationally linked electronic health records.
Over the past three years, his work shone a light on the prevalence, incidence and outcomes of cardiovascular diseases in homeless individuals. He also provided early modelling to inform the initial Covid-19 response.
Professor Banerjee, who is the chief investigator of the STIMULATE-ICP long-Covid study, shares more about his research projects and why the trend of using data from electronic patient records to predict outcomes and prognosis is here to stay.
As a cardiovascular doctor and researcher, I’ve got no business working in infectious diseases. However, early in the pandemic we found out there was a high risk of dying from Covid-19 or being admitted to a hospital or intensive care with Covid-19 if you’re older or if you have a chronic disease such as cardiovascular disease or diabetes. I became interested because my patients were asking me, ‘why am I more at risk and how much is that risk?’.
The IHI and UCL are part of Health Data Research UK – the UK’s national institute for health data science. We were able to work together to look at national level health records for certain diseases.
We did some very quick modelling at the beginning of the pandemic using electronic health record data on the risk of underlying conditions. Our analyses were done before the first UK lockdown and informed Government decision-making.
We showed that if the infection rate reached 10% in the first pandemic, we’d have 70,000 deaths. In fact, we underestimated this, as there were nearly 120,000 deaths in the first year of the pandemic.
Since then, we’ve carried on doing lots of different analyses around Covid, whether it’s on vaccinations, inequalities or underlying cardiovascular disease.
STIMULATE-ICP (Symptoms, Trajectory, Inequalities and Management: Understanding Long-Covid to Address and Transform Existing Integrated Care Pathways) is a multi-pronged approach to finding out more about the disease and is the largest clinical study of long-Covid to date over two years.
In the UK, an estimated two million people have experienced long-COVID symptoms lasting four weeks or more. Initially, scientists and politicians focused on the short-term impact of the virus. This research aims to improve care for chronically ill patients and deliver knowledge and evidence to clinicians, scientists and policymakers while collecting real-world data at scale. More than 50 researchers, health professionals, patients and industry partners from over 30 organisations are involved. The team spans primary care and specialist services, epidemiology, mental health and health economics. It also includes four patient groups who helped develop the research proposals.
We’re examining how people with long-Covid progress and recover and how healthcare resources such as investigations and rehabilitation are being used. We’re also exploring health inequalities and comparing them with other long-term conditions. We aim to recruit 4,500 individuals with long-Covid.
Among the care pathways being trialled are a multi-organ MRI scan and a digitally enhanced rehabilitation programme. This means that individuals can access information and rehabilitation via a purpose-built app ‘Living with Covid Recovery’. We’re also looking at how drugs can be potentially repurposed to treat long-Covid.
We expect preliminary results late in 2023.
The idea for this research arose because the existing published literature tended to focus on practical clinical crisis management for when this cohort became acutely sick, as well as drugs, alcohol and hypothermia. But there was not enough thought about chronic disease in this population.
Our study used primary care data collected between 1998 and 2019 to compare 8,482 homeless individuals with 32,134 housed people. They were matched by age and gender and lived in the same general practice area.
We found that homeless adults were 1.8 times more likely to have pre-existing cardiovascular diseases compared to other adults, putting them at higher risk of severe Covid-19 and early death.
We were piggybacking on a mobile screening service originally set up for tuberculosis screening and increasing rates of flu vaccination. Essentially, a mobile van drives around hostels and street locations in University College London Hospitals NHS Trust’s Find and Treat Service. We introduce clinical cardiovascular checks for cholesterol and blood sugar, and we’ve shown there’s a high rate of undiagnosed risk factors. We’re now looking to scale this up.
When I started my career, most of my work used large datasets. These were often research cohorts or registries and not from routine care at large scale. Now we work with hospitals and local primary care where research is based almost 100% on electronic health records.
I’m currently working on a heart failure project examining large scale electronic health records to see if there are different ways to subtype people who have different types of heart failure that are identifying by machine learning. Traditionally, images show how a particular part of the heart is functioning, which is a way of telling people what type of heart failure they have. I’m looking to see if there are other links that we haven’t found and subtyping people to see if that will predict their outcome or prognosis.
There are many advantages to using electronic patient data. First, data are more generalisable to the actual population and therefore findings are more likely to be relevant to the whole population.
Second, the coding of diseases and their risk factors can lead to standardised methods across studies.
Third, this type of data is more likely to create an ‘open science’ culture where our health data is seen as a public good.
Fourth, if more electronic health record research is done, there is less need for developing bespoke research cohorts, which are not efficient across individual diseases, settings and countries.
Amitava Banerjee is an advisory board member for HHE Clinical Excellence in Cardiovascular Care. He will be chairing two sessions at the event on 10 May 2023. Find out more and register for free here.
1st July 2020