This website is intended for healthcare professionals only.
Take a look at a selection of our recent media coverage:
26th June 2023
People in Ireland lead longer and healthier lives than most other Europeans, although behavioural risk factors, including smoking and obesity, remain important public health concerns. Quality of healthcare is generally good, but access to services is constrained by costs and waiting times.
The Covid-19 pandemic exposed health system weaknesses – in particular a shortage of health workers in the public sector and low intensive care unit capacity in public hospitals. It also revealed some of Ireland’s strengths in responding to crises, including the ability to develop technological solutions and to mobilise additional funding rapidly for health reform, health workforce and hospital resources.
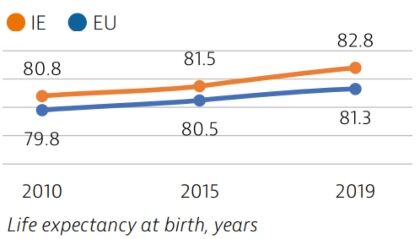
Life expectancy in Ireland has increased rapidly since 2000, reaching 82.8 years in 2019, 1.5 years higher than the EU average. Circulatory diseases and cancers remain the leading causes of death, accounting for more than 30% of all deaths.
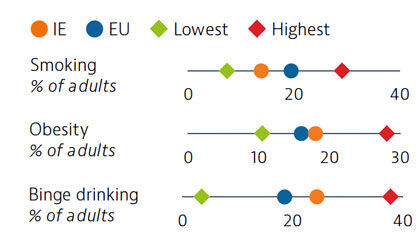
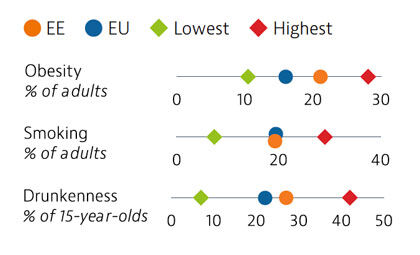
Behavioural risk factors are a major driver of mortality in Ireland. While smoking rates among adults have reduced, obesity among adults is on the rise and is now slightly higher than the EU average. One quarter of adults in Ireland report regular heavy alcohol consumption, which is also above the EU average.
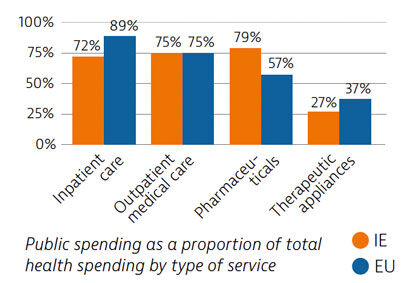
Spending on health per capita in Ireland is close to the EU average. Public coverage of spending for inpatient care is more limited than in other EU countries, while it is greater for pharmaceuticals. The majority of the population pays the full cost of general practitioner visits, outpatient prescriptions up to monthly thresholds, outpatient medical supplies and dental care. Spending on prevention was below the EU average in 2019 but saw a substantial increase in response to Covid-19.
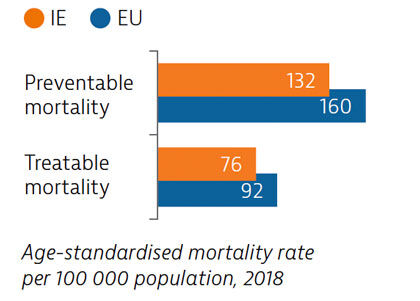
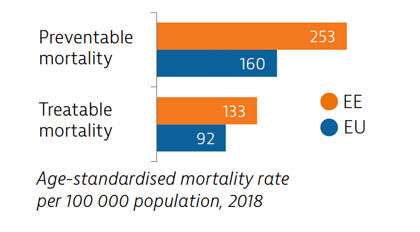
Mortality from preventable and treatable causes in Ireland is lower than in most EU countries. Still, there is room for further progress to reduce premature deaths through public health interventions and more timely diagnosis and treatment.
Covid-19 has affected access to care in Ireland: one fifth of the population reported unmet needs for medical care and treatment in 2020. Use of teleconsultations during the first wave of the pandemic aimed to improve access, and uptake was greater than the EU average.
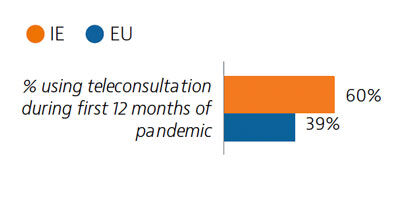
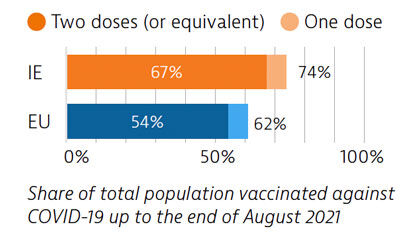
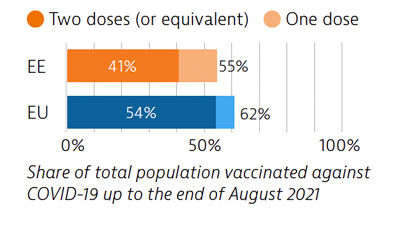
Ireland’s successful management in the early phases of the Covid-19 pandemic was challenged in late 2020 a severe third wave was experienced. By the end of August 2021, Ireland’s vaccination programme achieved above EU average results, with almost 70% of the total population receiving two doses (or equivalent).
OECD/European Observatory on Health Systems and Policies (2021), Ireland: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels.
23rd June 2023
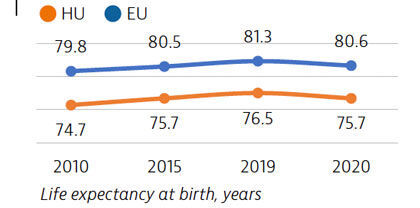
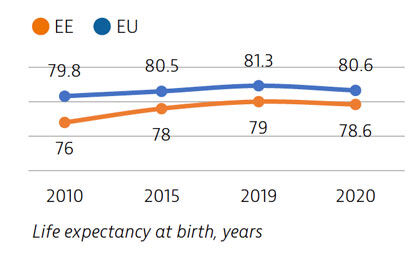
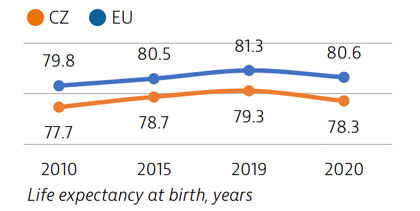
Life expectancy in Hungary increased fairly steadily before the Covid-19 pandemic, yet it remains almost five years below the EU average. Between 2019 and 2020, life expectancy fell temporarily by nearly 10 months because of the Covid-19 pandemic, a reduction similar to the EU average.
To maintain care continuity throughout the pandemic, new regulations on telehealth were introduced; nevertheless, levels of unmet medical needs rose. In response to persistent workforce shortages, in 2020, the government announced a new public sector employment contract, including a 120% pay increase for doctors by 2023.
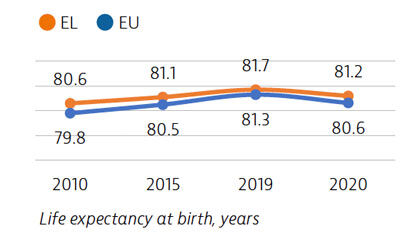
Life expectancy in Hungary grew by nearly two years between 2010 and 2019, before temporarily falling by 10 months in 2020 as a result of the Covid-19 pandemic, roughly the same reduction as in the EU overall. In 2020, the average person in Hungary lived nearly five years less than the EU average.
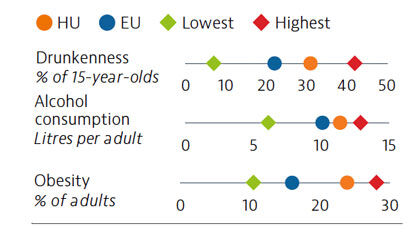
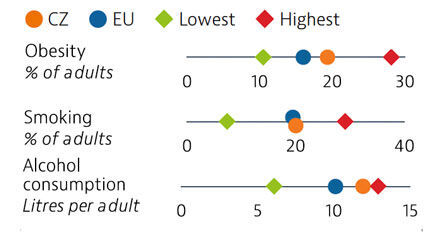
Behavioural risk factors account for approximately 50% of all deaths in Hungary. Compared to other EU countries, Hungary has relatively high levels of excessive alcohol consumption among both adolescents and adults. The proportion of adults who are obese is also greater than the EU average.
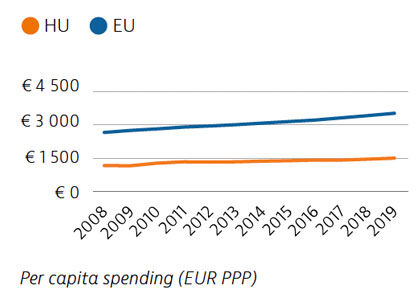
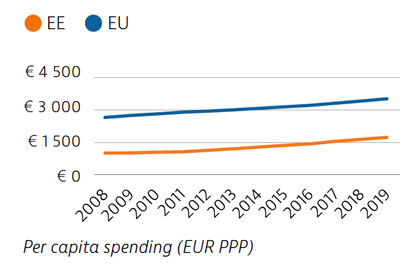
Health spending in Hungary increased at a moderate rate in the years before the pandemic, but remains below the EU average both in terms of spending per capita and as a percentage of GDP. Public funding accounts for two thirds of all health care spending, which is below the EU average of 80%, leading to high levels of out-of-pocket spending. During the pandemic, the government introduced substantial wage increases to stem the outflow of health professionals from the public sector.
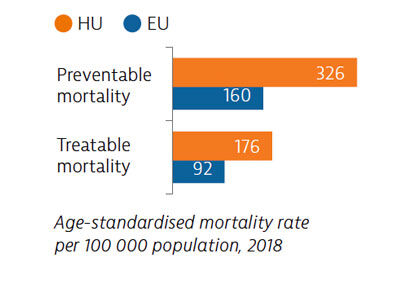
Mortality rates from preventable causes in Hungary were the highest of any EU country before the pandemic, highlighting the need to reduce behavioural and other risk factors. Deaths from treatable causes were also far above the EU average, reflecting issues with the quality of health services.
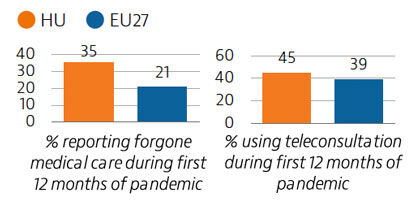
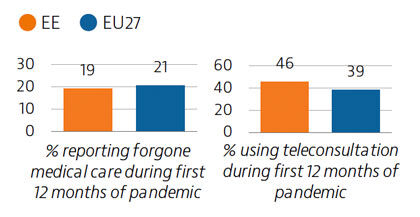
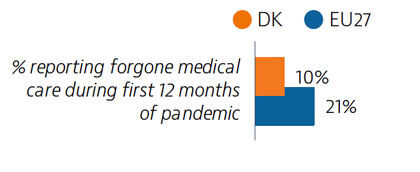
Levels of unmet medical needs are low in Hungary but rose temporarily in 2020: within the first 12 months of the pandemic, one in three people recorded unmet needs compared to one in five across the EU as a whole. Telemedicine facilitated access to care during the pandemic, with 45% of people attending a consultation online compared to 39% for the EU average.
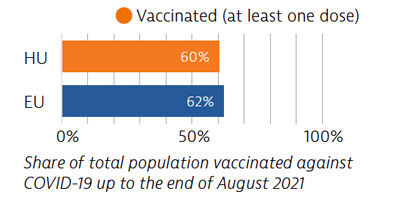
The number of workers and hospital beds increased to cope with pandemic demands. Simultaneously, the country introduced polices to free up existing resources, such as reserving a proportion of hospital beds for Covid-19 patients, resulting in delayed care for some non-Covid patients. Vaccination rates were relatively high at the beginning of the rollout but slowed afterwards.
OECD/European Observatory on Health Systems and Policies (2021), Hungary: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels.
Overall, the population in Greece enjoys good health, with a higher life expectancy than the European average. Extensive health system reforms have been ongoing since 2010, including the strengthening and expansion of publicly provided primary care services.
There has also been reinvigorated focus on prevention and tackling risk factors through a new national public health plan. Challenges remain in ensuring accessibility and affordability of care, particularly in the light of high out-of-pocket payments and the impacts of the pandemic.
Life expectancy in Greece in 2020 was about half a year higher than the EU average, although it fell temporarily by six months between 2019 and 2020 because of deaths due to Covid-19. The leading causes of death in 2018 were ischaemic heart disease, stroke and lung cancer. Prior to the pandemic, self-reported good health among the population was high, but Greek adults reported higher psychological distress than the EU average.
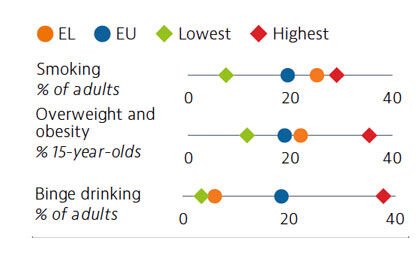
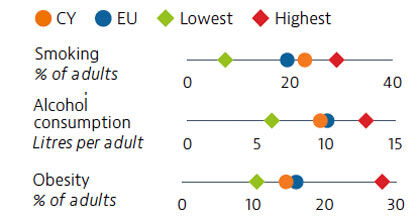
One in four adults is a daily smoker in Greece – one of the highest rates in the EU. Although tobacco smoking rates for 15-year-olds are lower than for adults, the growing popularity of e-cigarettes is a cause for concern. Adult obesity rates are equal to the EU average, but prevalence of childhood obesity has been growing steadily. In contrast, Greece has among the lowest binge drinking rates for adults in the EU.
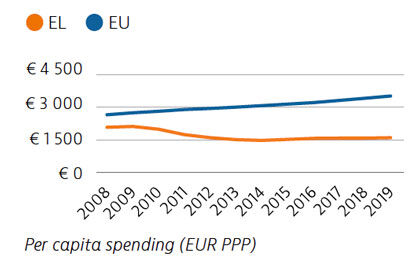
Per capita health expenditure in Greece (€1,603) continues to be well below the EU average. This equates to 7.8% of GDP, compared to 9.9% in the EU in 2019. Just under 60% of Greece’s health spending comes from public sources, while a very large share (35%) is paid out-of-pocket by households, mostly as co-payments for pharmaceuticals and direct payments for services outside the benefits package.
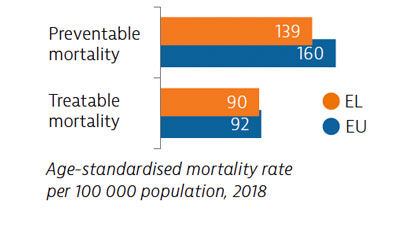
Mortality from preventable causes has remained stable in recent years and is lower than the EU average. New public health and prevention initiatives may help to reduce rates in the future. Greece also has slightly lower mortality from treatable causes than the EU average. New care co-ordination initiatives aim to improve detection and timely treatment.
Despite declines since 2016, Greece recorded the second highest level of unmet needs for medical care before the Covid-19 pandemic. Around one in four people reported forgoing care during the first 12 months of the pandemic. Teleconsultations have been used to maintain access to services.
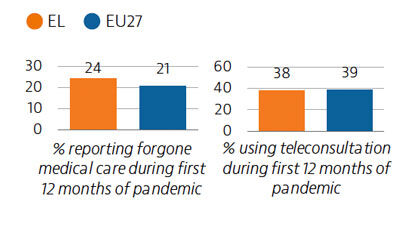
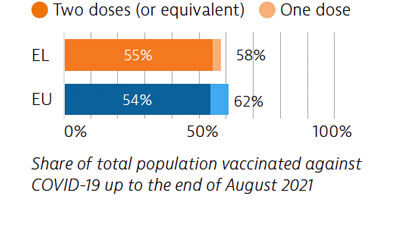
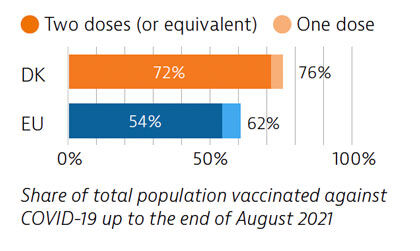
To meet the demands presented by the Covid-19 crisis, Greece upscaled laboratory and intensive care unit bed capacities, along with the health workforce and disease surveillance. After a slow start, the vaccination rollout accelerated, with 55% of the population receiving two doses by the end of August 2021.
OECD/European Observatory on Health Systems and Policies (2021), Greece: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels.
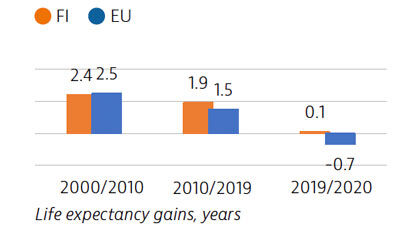
The Finnish population has seen improvements in life expectancy over the past two decades, and this positive development continued in 2020 despite the Covid-19 pandemic, as the government adopted a hybrid strategy to reduce the spread of the virus and protect high-risk people.
However, an ageing society and high numbers of people with chronic diseases and disabilities will raise the demand on health and long-term care systems in the future.
A recently approved major reform includes greater centralisation of responsibilities and resources at the regional level to improve access to care while controlling costs.
Over the past decade, life expectancy in Finland has increased at a faster rate than the EU average. Finland and Denmark were the only EU countries where life expectancy increased in 2020, although the gains were modest. Finland reported the lowest rate of Covid-19 cases and deaths among EU countries in 2020.
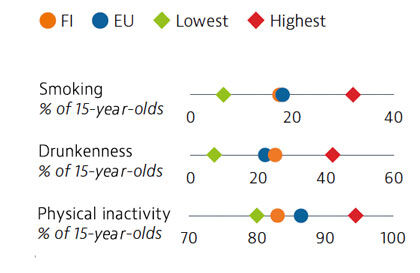
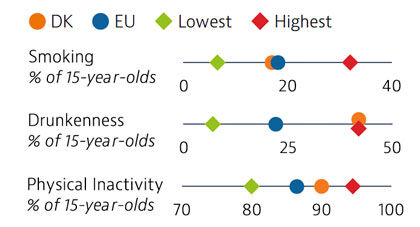
Daily smoking among adults in Finland has halved since 2000. Alcohol consumption has also decreased over the past two decades, although heavy episodic alcohol consumption remains more common in Finland than the EU average. Among young people, smoking and drunkenness rates are near the EU average. While physical inactivity among adolescents is only slightly lower in Finland than in the rest of the EU as whole, over 80% of adolescents are not doing sufficient physical activity every day.
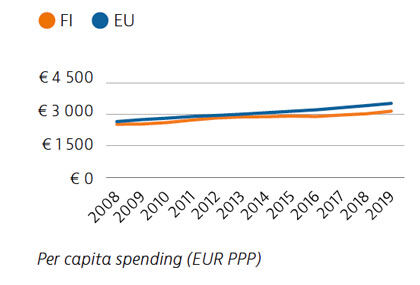
Health spending per capita in Finland increased at a very slow rate between 2013 and 2019. At €3,150 in 2019, it was over 10% lower than the EU average (€3,520). Health spending accounted for 9.2% of Finland’s GDP – almost one percentage point below the EU average of 9.9%. Public funding accounts for 78% of all health spending, which is a slightly lower share than the EU average (80%). In 2020 and 2021, the government provided additional funding of €4bn in response to the Covid-19 pandemic.
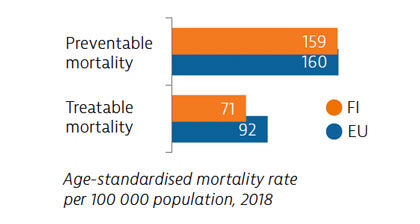
Mortality from treatable causes in Finland in 2018 was lower than the EU average, signalling that the healthcare system performs well in saving the lives of people with potentially fatal conditions. However, mortality that may be avoided through prevention policies was only close to the EU average.
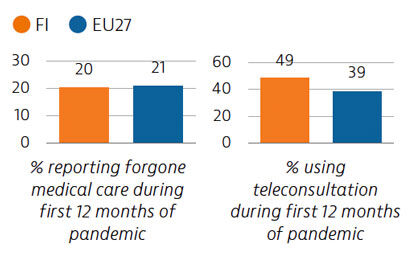
During the first twelve months of the Covid-19 pandemic, 20% of Finns reported unmet needs for medical care, which is close to the EU average. As in many other EU countries, the use of teleconsultations increased quickly during the pandemic to maintain access to care.
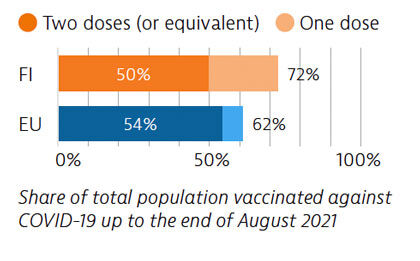
Finland followed a hybrid strategy to fight Covid-19, based on implementing targeted restrictions and a strong testing and tracing system. By the end of August 2021, more than 70% of the population had received a first dose, but only 50% had received two doses or the equivalent.
OECD/European Observatory on Health Systems and Policies (2021), Finland: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels.
The life expectancy in Estonia has grown strongly over the last two decades. However, while the health status of the population has been getting closer to the EU average since 2001, aggregate numbers obscure inequalities by region, gender and socioeconomic group.
Compared to most other EU countries, Estonia spends less on health care, and although direct government transfers were injected into the system to address the Covid-19 pandemic, the health system remains chronically underfinanced.
As a leader in e-health, Estonia’s health system has been able to effectively support a variety of pandemic response measures and to deliver health services.
Since 2000, Estonia’s life expectancy has increased more than any other EU country, although it fell by 0.4 years between 2019 and 2020 due to the Covid-19 pandemic. On average, women live 8.5 years longer than men; this gap in life expectancy by gender is much greater than the EU average of 5.6 years. Sizeable health inequalities also exist across income levels, regions and education.
Behavioural risk factors accounted for nearly two fifths of all deaths in Estonia in 2019. Overweight and obesity are a growing concern. More than one in five Estonian adults is obese, and obesity is increasingly common among adolescents. Smoking rates have been decreasing, but nearly 20% of adults still smoke daily. Similarly, alcohol consumption has declined overall but is still high for adult men and adolescents.
In per capita terms, spending on health in 2019 was €1,733, which is less than half the EU average. Total health expenditure was also significantly lower when measured as a share of GDP (6.7% compared to an average of 9.9% of GDP in the EU). Around three quarters of health spending in Estonia comes from public sources, with one quarter from out-of-pocket payments – mostly for medicines and dental care.
Both preventable and treatable mortality are higher in Estonia than the EU averages, but they have decreased substantially since 2012. Ischaemic heart disease remains one of the leading causes of avoidable deaths. Estonia has lower avoidable hospital admissions for chronic diseases than many other EU countries.
Before the pandemic, Estonia’s population reported the highest level of unmet medical needs in the EU. During the Covid-19 crisis, reported unmet needs were higher than usual, but the rapid uptake of remote consultations supported by existing digital infrastructure helped to maintain access to care.
Estonia leveraged its extensive digital infrastructure to respond to the Covid-19 pandemic, including for testing and contact tracing. Digital tools also facilitated the rollout of the Covid-19 vaccination programme, with 41% of the population receiving two doses (or equivalent) by end August 2021.
OECD/European Observatory on Health Systems and Policies (2021), Estonia: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels.
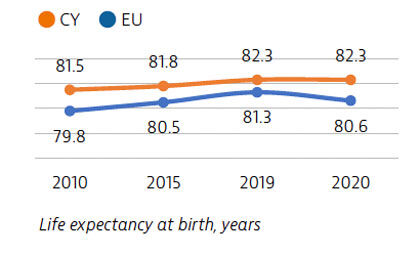
Overall, the Cypriot population is among the healthiest in the EU. As of August 2021, the impact of Covid-19 on mortality and life expectancy had been limited. The population enjoys good health outcomes, despite the prevalence of risk factors such as smoking and obesity.
Since 2019, health system reforms to introduce universal coverage and improve overall efficiency have been implemented, despite the ongoing pandemic, and changes to healthcare financing mechanisms have facilitated surge capacity.
As well as improving coverage and resilience, the new General Healthcare System is expected to improve accessibility by cutting waiting times.
As in several other EU countries, gains in life expectancy in Cyprus slowed over the past decade. Notwithstanding the Covid-19 pandemic, life expectancy in 2020 remained stable at 82.3 years. The leading causes of death are circulatory diseases, cancer and diabetes. While the number of people dying from circulatory diseases has consistently fallen since 2015, the cancer mortality rate has remained stable.
Smoking rates in Cyprus are among the highest in the EU and constitute a major public health issue. Although adult obesity rates are close to the EU average, childhood obesity is increasingly common. Alcohol consumption is less of a concern, but all the risk factors are more prevalent in lower-income households, contributing to health inequalities.
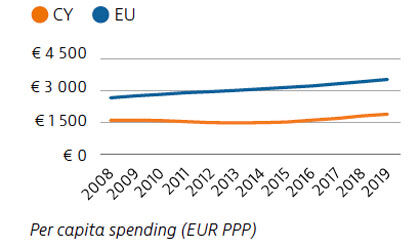
Spending on health in Cyprus remains consistently below the EU average, at €1,881 per capita in 2019 compared with €3,523 for the EU as a whole. Spending on all components of the system is low. One important goal of recent extensive health system reforms to introduce universal coverage is to reduce what was the highest level of out-of-pocket spending in the EU by improving financial protection.
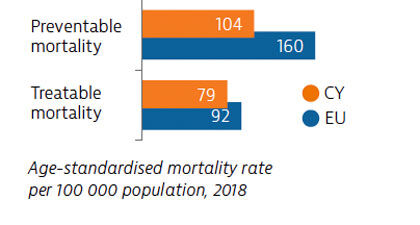
Death rates from preventable causes in Cyprus are among the lowest in the EU. The leading cause of preventable mortality is lung cancer, driven by high smoking rates. Death rates from treatable causes are also below the EU average. Strategies are in place to improve comprehensive data collection on cancer survival rates.
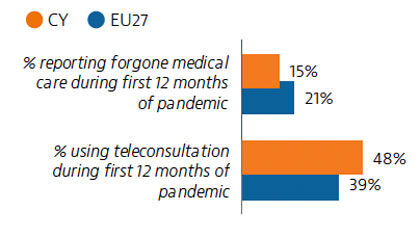
Fewer than one in six Cypriots reported having forgone necessary medical care during the Covid-19 pandemic, a rate consistent with the below-average rates of unmet medical needs reported before the pandemic across the EU. To ensure safe access to care during the pandemic, patients were encouraged to access their doctor primarily by telephone.
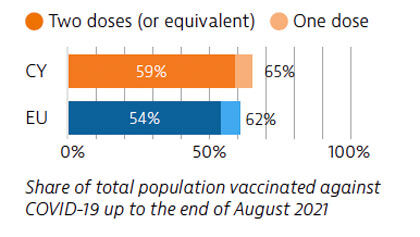
Financing reforms introduced shortly before the pandemic allowed greater flexibility in planning and contracting with service providers. This facilitated the development of surge capacity during the Covid-19 crisis. Cyprus was also able to roll out its vaccination campaign swiftly. The main capacity constraint is the ongoing shortage of health workers.
OECD/European Observatory on Health Systems and Policies (2021), Cyprus: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels.
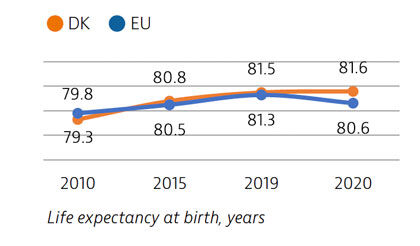
Life expectancy in Denmark in 2020 was one year higher than the EU average, partly because the number of Covid-19 deaths was much lower than in most other EU countries. Denmark quickly scaled up its testing capacity at the beginning of the pandemic, which enabled effective detection, tracing and isolation of confirmed cases early on.
Rapid implementation of teleconsultations and lower than expected pressure on designated Covid-19 capacity ensured relatively low unmet needs during the pandemic.
Life expectancy in Denmark has increased more rapidly than the EU average since 2010 and continued to grow at least slightly in 2020, while it fell significantly in most EU countries because of Covid-19. Seven in 10 Danes report being in good health, which is similar to the EU average. However, non-negligible socioeconomic differences in health status persist.
Smoking rates among both adults and adolescents have reduced sharply over the past two decades, and are now below the EU average. However, adolescents in Denmark drink more alcohol than their Nordic and EU peers. High rates of physical inactivity among adolescents are becoming an important public health issue.
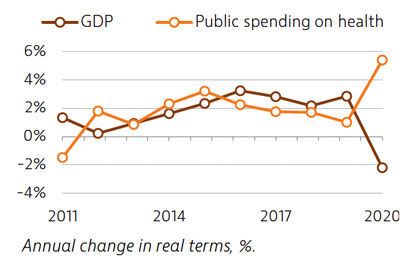
Spending on health in Denmark has remained slightly above the EU average over the past decade. Health expenditure grew at an average rate of 2% per year in real terms between 2015 and 2019 – slightly slower than the EU average. As a result of the Covid-19 pandemic, public spending on health increased by over 5% in 2020, while GDP fell by more than 2%, temporarily increasing the health spending share of GDP.
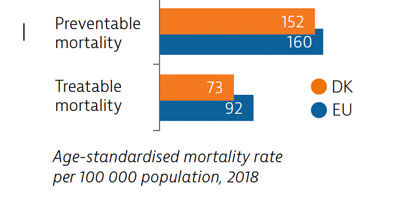
Mortality rates from preventable causes in Denmark in 2018 were close to the EU average. Lung cancer is the leading cause of preventable death – a legacy of high smoking rates among previous generations. Mortality rates from treatable causes are below the EU average, although higher than in Sweden and Norway.
Danes reported low levels of unmet needs before the pandemic. During the first 12 months of the pandemic, levels of unmet needs were also lower than the EU average. Rapid expansion of telehealth ensured continuity of ambulatory care, but non-essential and elective care were delayed during the peaks of the first and second waves to free up hospital capacity for Covid-19 patients.
Up to the end of August 2021, Denmark experienced 3.5-times fewer Covid-19 deaths relative to its population size than the EU average, although the Covid-19 death rate was higher than in Finland and Norway. As of the end of August 2021, 72% of the Danish population had received two doses of the Covid-19 vaccine or equivalent – a proportion higher than the EU average.
OECD/European Observatory on Health Systems and Policies (2021), Denmark: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels.
Although Czechia spends considerably less on health than most other EU countries, its health system provides a broad benefits package and reported unmet needs for medical care are low. In 2020, life expectancy in Czechia was more than two years below the EU average, after the Covid-19 pandemic led to a temporary reduction of one year compared to 2019.
The pandemic response highlighted areas for improvement in crisis preparedness and workforce capacity, especially in some regions. The financing decisions made during 2020 alleviated the short-term financial pressure on the system.
Life expectancy in Czechia steadily improved over the last 10 years and in 2019 was two years below the EU average. However, the Covid-19 pandemic temporarily set the country back to 2013 levels – a larger impact than in many other EU countries.
Nearly half of all deaths in Czechia in 2019 could be attributed to behavioural risk factors – particularly poor diet, smoking and alcohol consumption. Obesity rates have steadily increased over the past 15 years and are now around 20% for adults, contributing to high prevalence of diabetes and other diet-related diseases. Alcohol consumption is among the highest in the EU.
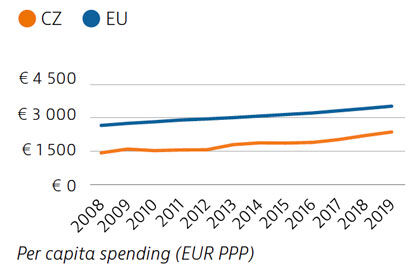
Czechia’s health expenditure in 2019 was 7.8% of GDP and €2,362 per capita – both substantially below the EU averages (9.9% and €3,521). Most health expenditure is financed from public sources, predominantly through the compulsory insurance system. Czechia significantly increased contributions from the state budget into the insurance system to cover almost all pandemic-related expenses.
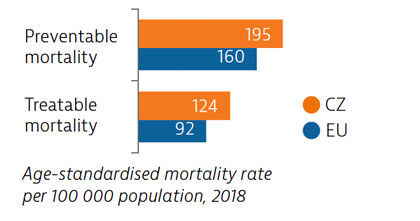
Despite steady decreases over the past decade, Czechia still had relatively high levels of preventable and treatable mortality before the pandemic. Additional investment in public health interventions and in incentivising healthier habits among the population could help achieve further progress. Cancer survival rates are now close to the EU average, but Covid-19 led to a temporary drop in activity such as screening, which could set back this advance.
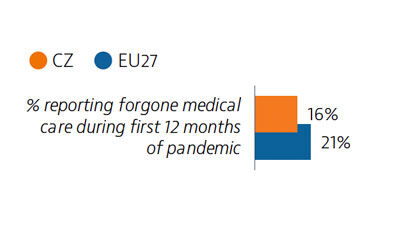
Prior to 2020, Czechia had one of the lowest levels of unmet needs for medical care in the EU, although some informational barriers to care existed. During the first wave of the pandemic, health services were less disrupted than in the EU overall (16% of Czechs reported having forgone medical care).
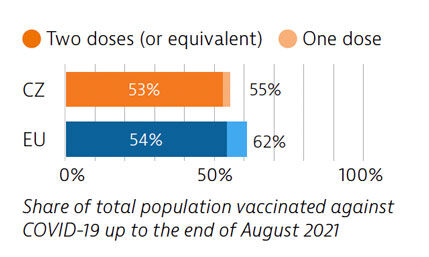
Czechia contained the first Covid-19 wave but struggled to slow down the second wave, partly due to limited planning capabilities and insufficient clarity in its public communication. By the end of August 2021, 16% of the population had been diagnosed with Covid-19 (compared to 8% across the EU), while over half of the population (53%) had been vaccinated with two doses (or equivalent).
OECD/European Observatory on Health Systems and Policies (2021), Czechia: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels.
Life expectancy in Croatia remains below the EU average and temporarily declined in 2020 as a result of deaths that occurred during the Covid-19 pandemic. Although the Croatian health system provides equitable access to a broad range of services, unmet needs are likely to have increased during the pandemic.
With a sufficient level of physical infrastructure and number of health workers, Croatia responded quickly to the first wave of the Covid-19 pandemic but was more hesitant to reimpose stringent measures in subsequent waves.
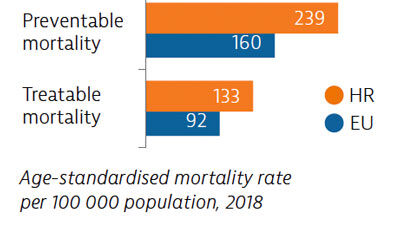
Rates of preventable and treatable mortality before the pandemic were comparatively high, suggesting scope for strengthening public health policies and improving healthcare.
Life expectancy in Croatia in 2020 was almost three years below the EU average. One of the reasons for this persistent gap is that Croatia has one of the highest mortality rates from cancer in the EU. In 2020, Covid-19 became the third leading cause of mortality. Life expectancy temporarily fell by just over nine and a half months between 2019 and 2020, reaching 77.8 years, slightly more than the average drop across the EU.

Croatia has much scope to address modifiable health risk factors, including unhealthy diets, tobacco smoking, alcohol consumption and low physical activity. Smoking rates among adults are high, adolescent smoking is among the highest in the EU and the proportion of people who are obese is also high.
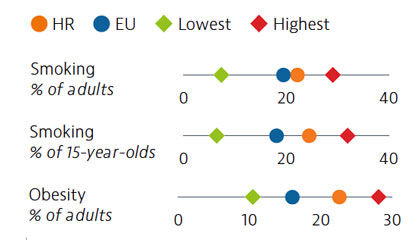
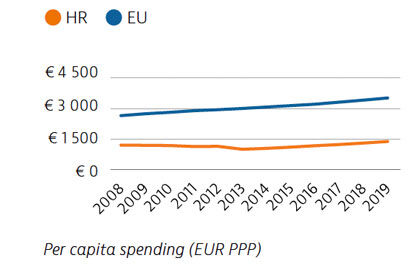
Health spending per capita is lower in Croatia than in most other EU countries, and has remained fairly constant in recent years. However, public funding as a proportion of total expenditure was 81.9% in 2019 – higher than in most EU countries with comparative levels of expenditure. The share of public financing was higher than the EU average for all areas of care, with a higher proportion of public coverage in particular for dental care and pharmaceuticals.
Mortality rates from preventable and treatable causes in Croatia are far above the EU average. This is due in part to weak intersectoral policies to address key determinants of ill health, such as smoking and poor nutrition, as well as to shortcomings in providing timely and effective care.
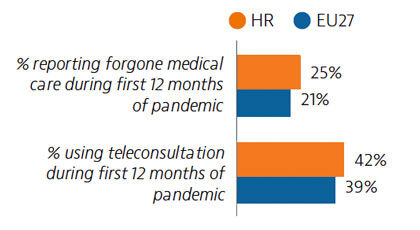
During the first 12 months of the pandemic, a considerable share of people reported unmet needs for medical care. However, a higher proportion than in the EU overall resorted to teleconsultations as a means of accessing services.
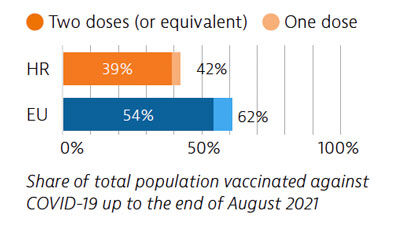
During the first wave of the pandemic, Croatia quickly implemented containment measures and scaled up resources. It was harder hit by the second wave. By the end of August 2021, 42% of the population had received at least one dose of a Covid-19 vaccine.
OECD/European Observatory on Health Systems and Policies (2021), Croatia: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels.
14th June 2023
Life expectancy in Italy is among the highest in Europe, but it fell at least temporarily in 2020 because of deaths due to Covid-19. While the Italian health system generally provides good access to high-quality care, the pandemic highlighted important structural weaknesses, including years of low investment in the health workforce and the health information infrastructure.
The pandemic stimulated many innovative practices in Italy, such as the rollout of special units for continuity of care, which could be expanded to build a more resilient healthcare system.
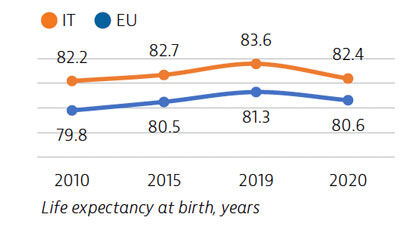
Life expectancy in Italy in 2020 was almost two years higher than the EU average, but it fell by 1.2 years because of deaths due to Covid-19. Even before the pandemic, gains in life expectancy had slowed considerably since 2010 compared with previous decades, partly due to increased mortality rates from respiratory diseases among older people.
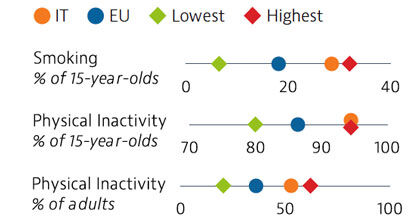
Risk factors for health are major drivers of mortality in Italy. While tobacco consumption has fallen among adults over the past decade, nearly 30% of 15-year-olds reported that they had smoked in the past month in 2018. Physical inactivity among both adolescents and adults is also relatively high in Italy, contributing to overweight and obesity.
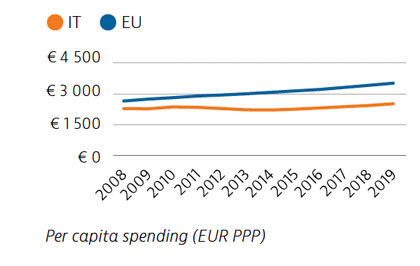
Spending on health in Italy grew slowly in the decade before the pandemic. In 2019, health expenditure was substantially lower than the EU average, both in per capita terms and as a share of GDP. About 74% of health spending was publicly funded in 2019 – a lower share than the EU average of 80%. In response to the Covid-19 pandemic, the Italian government allocated additional funding of €3.7bn in 2020 and €1.7bn in 2021 to the health system – an increase of 3.3% and 1.7% over the original funding plan.
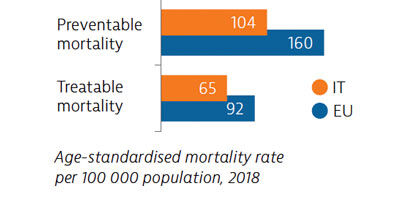
Mortality from preventable and treatable causes was lower in Italy than the EU average in 2018, indicating lower prevalence of many risk factors to health compared to the rest of the EU and a healthcare system that is generally effective in treating patients with life-threatening conditions.
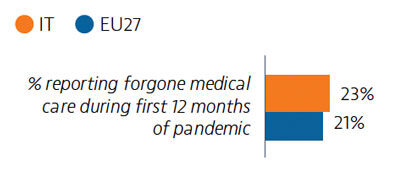
Although access to health care is generally good in Italy, the Covid-19 pandemic significantly hampered access to care: 23% of the population reported some forgone care during the first 12 months of the pandemic – slightly more than the EU average of 21%.
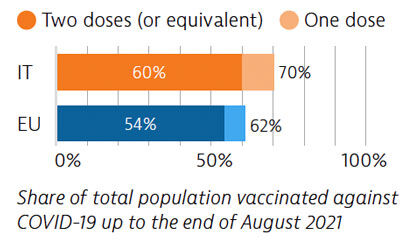
Italy was among the EU countries hardest hit by Covid-19 in terms of death rates, particularly during the first wave. Like other EU countries, Italy accelerated its vaccination campaign in the first half of 2021 as the main way out of the pandemic, while continuing to implement other measures to protect its population and reduce pressure on its hospitals.
OECD/European Observatory on Health Systems and Policies (2021), Italy: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels