HOPE representatives provide information on the most significant changes that have happened in their respective countries in 2016 and their main expectations for 2017
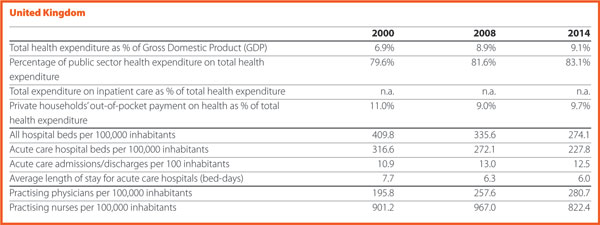
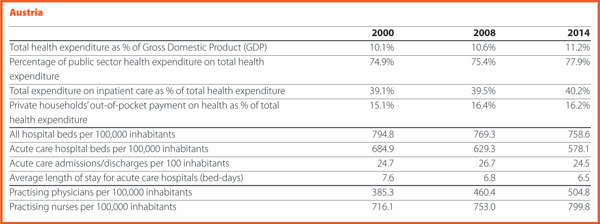
Austria

Nikolaus Koller HOPE Governor

Ulrike Schermann-Richter Head of department, Federal Ministry of Health and Women’s Affairs
Could you present the two/three main changes that happened in the hospital and healthcare sector in your country in 2016?
After almost ten years of basic work and preparation, the implementation of the Electronic Health Record (ELGA) has started. ELGA is a system for the standardisation of electronic communication between healthcare providers and for the networking of health data and information. It offers patients, doctors, hospitals, care facilities and pharmacies access to medical findings, discharge letters and current medication data regardless of the timing and the place where such data has been produced. ELGA aims at improving treatment quality and increasing patient safety as well as patient autonomy. The system will be rolled up until 2022. First, letters of discharge, as well as laboratory and radiological findings in public hospitals were made available via ELGA. Outpatient clinics, private hospitals and medical practitioners will gradually follow the implementation phase.
The Austrian healthcare system is traditionally hospital centred. Despite 30 years of continuous efforts, the country registers a high number of acute beds and rate of discharges per inhabitant. Many services are provided on an inpatient basis although they could have been offered as outpatient services.
The DGR-based hospital funding system (LKF- Leistungsorientierte Krankenanstaltenfinazierung) has been developed for the calculation of inpatient hospital costs and has been running since 1997. In 2016, the DRG system was not only subject to routine maintenance, but was further developed by complementing a nationwide calculation model for the hospital outpatient sector.
The focus is on those cases in which frequent inpatient admissions, not medically induced, were observed. The model to be applied by 2019 at the latest is intended to incentivise the hospitals to provide services in outpatient settings rather than inpatient ones.
Fewer incentives have been created by the new working time rules for hospitals, which had to be aligned with the requirements of the EU. The law stated a gradual reduction of the working hours by 2021. Salaries, however, have not been cut in the same proportion as working hours, thus the personnel costs increase in the intramural field which forces planners and providers to optimise the utilisation of the work force resources and care processes.
Could you present us the two/three expectations that you have for 2017?
The Austrian healthcare system is complex. It is publicly organised, but this organisation involves several levels of politics and public administration – the federal government, the nine provinces, districts and local authorities and the social insurance organisations. Coordination between the different sectors of the healthcare system and its actors is built on a legally defined form of cooperation, the so-called target-based health governance.
A ‘product’ of this cooperation is the National Framework for Healthcare Planning (ÖSG-Österreichischer Strukturplan Gesundheit); a tool for integrated healthcare planning that depicts all provision levels. The ÖSG is indeed a valuable planning basis but, being just a compilation of expert’s opinions on the state-of the art of healthcare provision, its specifications are only recommendations and not legally binding. After many years of efforts, a legal basis can now be created, offering the possibility to make planning specifications of the ÖSG binding for the extra and intramural sector by ordinance. In 2017, the parts of the ÖSG, which are indispensable for the sustainable provision of healthcare services, such as planning reference values and criteria, should be identified and made legally binding.
A major goal of the healthcare reform 2013, namely the reorganisation of primary healthcare and enhanced primary healthcare capacity including the target to have implemented multi-professional primary healthcare facilities for at least 1% of the population by the end of 2016, could not be achieved, mostly due to the massive opposition of the doctors’ chamber. However, the health reform package for the coming period 2017–2020 reaffirmed the strengthening of near-home and multi-professional primary healthcare and devoted 200 million Euros for this purpose. “We are confidant that the relevant legal base will be decided in the foreseeable future and that these provision model can finally be implemented in Austria”.
This is intended to make the working environment in the public healthcare system more attractive and to provide a better work-life balance for healthcare providers. Patients will be offered longer opening hours and more services and better coordination of different areas of treatment is to be ensured. This will reduce the burden on hospitals and their outpatient clinics.
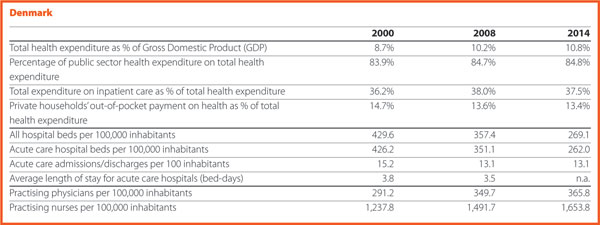
Denmark

Eva M Weinreich-Jensen HOPE Governor, Danish Regions
Could you present the two/three main changes that happened in the hospital and healthcare sector in your country in 2016?
In 2016, a new Danish Quality programme based on a close cooperation between the state, regions and municipalities have been launched. After ten years with the former quality programme, the sector, and especially the staff, felt that the focus was on processes and registration, that are not central aspects for the care of the patients. The new programme sets clearer goals about the improvement of results for the patients. “We said goodbye to accreditation in the hospitals and the prehospital area, and hello to a model where each hospital and region will be able to set their own goals based on the challenges they face, but still in the context of reaching eight new national goals. We have already come far to establish national learning and quality teams, that are meant to improve the clinical quality and result in specific areas and to improve the experience for the patients and relatives”. The sense that this is a mutual ambition between sectors sets the scene for a very positive development, embraced by patients, managers, staff and politicians.
Another import area of improvement in Denmark is value-based healthcare, an international trend that Denmark has become part of in 2016. For almost two decades, Denmark has increased activity with great success – patient waiting lists have been reduced significantly. Now it is time to shift focus towards achieving the best outcomes at the lowest cost – following the goal of the Danish value-based healthcare initiative. In the future, there will be more attention on spending resources more wisely, and on designing healthcare organisations around what creates value for the patients.
This is an ongoing transformation as hospitals in all the country are dealing with value-based healthcare. As part of the value-based healthcare initiative, medical staff and patients are identifying outcome-goals for seven patient groups; including apoplexy, prostate cancer and epilepsy. In the coming years methods for value-based healthcare will be tested in practice, and the initiative will work towards developing an information technology platform that can support it by connecting information about costs and patient outcomes. The concept of value-based healthcare is the road towards a more efficient and patient-oriented healthcare system.
Could you present us the two/three expectations that you have for 2017?
It is a clear ambition that our improvement work will be much more patient centred and focused on value for the patient. The expectation relies on starting closer with citizens, patients and carers.
However, it is needed to tear down some walls between hospital and society, in order to actively prevent health problems, and to help citizens taking an active role in their own health. New initiatives have been developed in this area. The synergy of all the initiatives taken will hopefully take place in 2017.
Finland

Aino-Liisa Oukka HOPE Governor, Director Oulu University Hospital
Could you present the two/three main changes that happened in the hospital and healthcare sector in your country in 2016?
As part of New Social and Welfare Reform, a change in the Healthcare Act was approved by the Parliament in December 2016. According to this, from January 2019, 18 counties, instead of municipalities and 20 hospital districts, will be responsible for organising social and healthcare services. The provision of primary care services will be opened to competition.
Moreover, all social and healthcare related investments must be evaluated and accepted by the Ministry until 2019, when the responsibility is transferred to the counties.
Finally, a web-based ‘Virtual Hospital’ digital service was established.
Could you present us the two/three expectations that you have for 2017?
The preparation of the New Social and Welfare Reform as well as on the Acts on the healthcare services financing will continue. Cancer centres, rare diseases centres and biobanks will be (re)organised and new joint realities formed. Discussions on patients and citizens’ rights and responsibilities in relation to society’s capabilities will (hopefully) advance.

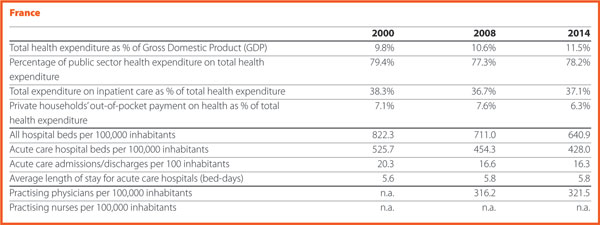
France

David Gruson HOPE Governor, Chief executive, French Hospital Federation

Yves-Jean Dupuis Chief executive, French Federation of Non-Profit Hospitals (FEHAP)

Pascale Flamant Chief executive, French Federation of Comprehensive Cancer Centres (UNICANCER)
Could you present the two/three main changes that happened in the hospital and healthcare sector in your country in 2016?
The first big change affecting the healthcare landscape in France in 2016 is the territorial reform reducing the number of the regions to 13. This reform sparked off a vast restructuration at the regional level concerning above all the Regional Health Agencies. These, with a bigger territory should adapt their missions at the regional scale together with all the stakeholders in the healthcare sector. A new Public health Agency was created (Santé Publique France). It is a merger of already existing agencies: the French Institute for Public Health Surveillance (InVS), the French Institute for Health Promotion and Health Education (Inpes) and the Establishment for Public Health Emergency Preparedness and Response (Eprus). The aim of this new entity is to serve the population in all aspects of public health based on scientific knowledge, data, and information. The country went through a health system reform, aiming for the ‘modernisation’ of the sector, with a movement of closer cooperation between the local stakeholders and particularly with the progressive merging of some resources between hospitals on the same territory. Moreover, in 2016 there was the launch of the Medical Genomic Plan 2025.
Could you present us the two/three expectations that you have for 2017?
(The reply to this question was provided in April 2017, before the presidential election). The presidential election will take place in April and May 2017. Unlike the previous campaigns, the health-related issues do have a place in the candidates’ programmes this year, and the candidates presented some proposals for the improvement of the French health system. The main expectation for 2017 is a better integration of healthcare and social care with a shift from hospital care to community care, and the strengthening of social care. This would permit the challenges the country is currently facing with the rise of chronic diseases along with the ageing of the population to be addressed. These chronic diseases are preventable through closer partnership among all the stakeholders within the health sector to achieve the realisation of the ‘health pathway’ for anyone. Finally, another expectation for 2017 is the promotion of the use of new technologies to support patients in their care. The new technologies are indeed opportunities to address the inequalities, to improve the quality and efficiency of the system.
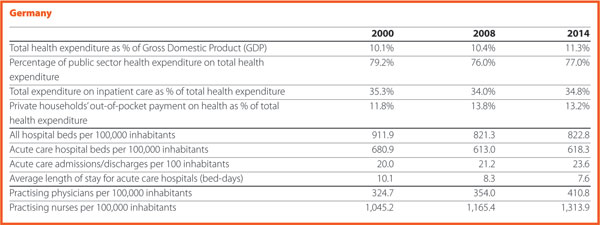
Germany

Georg Baum HOPE Governor, Chief executive, German Hospital Federation
Could you present the two/three main changes that happened in the hospital and healthcare sector in your country in 2016?
Hospital provisions and workforce present growing trends in 2016. Hospital reimbursements raised by 3%, thus 2.5 billion Euros in the same year. The main challenges are represented by the increasing wages and the failure of the investment delivery from the Federal States.
Recently, German hospitals have been working a lot on implementing the
Federal hospital act, which was finally released in late 2015. This act was mandating the partners of the self-government system in German healthcare (that is, hospitals, doctors, health insurance funds) to take major decisions in the Federal Joint Committee (GBA). Despite important steps have been taken, for example, by allowing further surcharges for hospital centres with special tasks, other tasks are pending for execution. The planned switch to a newly invented price-system for psychiatric care in hospitals is postponed and the actual budget system will remain in function so far.
Could you present us the two/three expectations that you have for 2017?
A major challenge for the near future will be the introduction of further instruments for insurance of quality. For this reason, the recently established Institute for Quality Assurance and Transparency in Healthcare (IQTiG) is, as a contractor of the GBA, developing the methodological basis for the inclusion of quality aspects when it comes to preparing the hospital plans by the Federal governments and for a better coordination of primary and secondary care. Moreover, further instruments have to be developed for quality assurance, for better quality of healthcare provision, for surcharges or deductions of fees in relation to quality of hospital care.
At EU level, German hospitals were and are supporting the strong opposition against standardisation of healthcare services. European standardisation bodies are exploring the healthcare field to create standards on services provision. A comprehensive alliance of EU stakeholder organisations, including hospitals, doctors, health insurance funds and social partners as well as governments of numerous EU Member States are opposing this development.
DKG is also open to contributing constructively to the evolving discussion to further develop Health Technology Assessment (HTA) at EU level. The European Commission is currently developing plans to compare HTA methodologies and procedures. It should be a common aim to improve HTA intelligence by sharing knowledge and experience. This could give support to the responsible Institutions in the Member States in good HTA decision making.
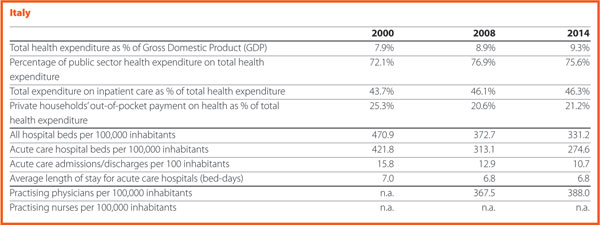
Italy

Domenico Mantoan HOPE Governor, General Director, Area Sanità e Sociale, Department for Health and Social Affairs, Veneto Region
Could you present the two/three main changes that happened in the hospital and healthcare sector in your country in 2016?
Could you present us the two/three expectations that you have for 2017?
In Italy, one of the most important matters is the approval by the Italian national Parliament of the new LEA – Essential Levels of Assistance – corresponding to the minimum levels of health services that have to be provided by the National Health System (NHS) through public funding. LEA update represents major news since the last time they were updated was 2001. This was due to the difficulty of finding public resources aimed at covering the cost of such update and the consequent increase of public healthcare expenditure. Meanwhile, some Regions were able to guarantee essential levels of assistance by means of regional laws and using regional funds. Some healthcare services included in LEA must be provided for free (that is, acute care hospital admission) while others need a co-payment from the patient. The cost of new national LEA is estimated at around 800 million per year, that is approximately 0.7% of the Italian National Health Fund (113 billion in 2017).
LEA regard hospital care, primary care, outpatients care, intermediate and home care and describe the main categories of treatments, diagnosis proceedings, health equipment covered by the Italian National Health System. They may refer both to pathological and physiological events (that is, pregnancy) and some of them have been foreseen also for preventive medicine.
LEA are stated considering basic criteria such as sustainability, patient safety, ethics (that is, aesthetic medicine is not covered). In particular, the legislation takes into account criteria of clinical validity (is the innovation result medically meaningful?), clinical utility (does the innovation improve healthcare?), analytical validity (is the innovative test accurate and reliable?). It states also the clinical situation for which the coverage is guaranteed and the appropriate prescription (that means appropriate utilisation of resources) becomes a key topic.
A National LEA Commission has been created with the task of monitoring the current LEA utilisation and suggesting their update, and to avoid waiting for a decade for the introduction of the new ones.
As regards the Veneto Region, the most recent matter is the approval of the Regional Healthcare Reform by the regional Parliament. This is based on two main topics: the reduction of the number of the Health Social Local Trusts (HSTLs) and the creation of an innovative Zero Trust (Azienda Zero).
HSLTs number decreases from 21 to 9 with the smallest HSLT (in term of residents) serving around 210,000 people (in the Dolomites mountainous area of Veneto Region), and the largest one serving around 930,000 people, in the central part of the Region, that is, in the most urbanised area. Research and Teaching Hospitals Trusts remain the same: two Teaching Hospitals and one Research and Care Trust.
The above mentioned decreasing HSLTs number was possible because a part of the HTLs functions shifted to the innovative Zero Trust, in which are centralised functions previously carried out by the different trusts. Its aim consists in increasing efficiency and productivity and in absorbing functions previously performed by some regional offices (that is, large procurement, regional part of risk management, regional education and training addressed to management, part of the accreditation system, HTA). This means a new distribution of competencies and personnel.
An interesting and important task for Zero Trust is the developing of a centralised ICT system, allowing the storage of health digital data in a unique archive. In this way patients and professionals could access to this kind of information regardless of the trust where it was registered.
In conclusion, the creation of Zero Trust appears as an important challenge for achieving higher healthcare levels, putting the focus on efficiency and sustainability.
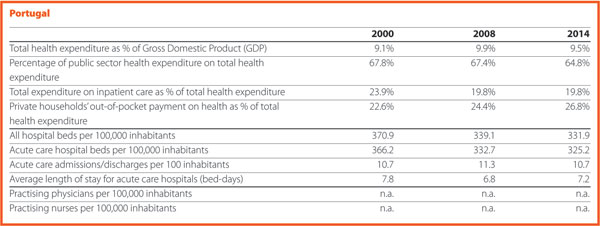
Portugal

Ana Escoval HOPE Governor, Portuguese Association for the Development of Hospitals
Could you present the two/three main changes that happened in the hospital and healthcare sector in your country in 2016?
In 2016 the National Health Service (SNS) in Portugal went through several structural changes, namely at the hospitals and primary care levels.
Within this framework, it is important to refer to the creation of the “Portal do SNS” – a web-portal of SNS designed within the “Simplex” Programme in February 2016. This platform allows the access to a wide collection of data and to on-line services, organized in four major areas – SNS, Institutional, Citizen, Professionals – which are made available by the Institutions within the SNS and competent bodies within the Ministry of Health. This web portal stands by transparency and intends to facilitate the communication, by aggregating all of the relevant information regarding the SNS, bringing closer the different audiences of the Ministry of Health.
This web platform is extremely relevant, allowing a new form of communicating with citizens, more transparent and accessible. It can perform many different tasks such as to schedule an on-line appointment, to renew the prescription of drugs (when reported in the system by the family doctor), make the ‘Testamento vital’ (the living will where the patient expresses his/her treatment or healthcare preferences if unable to decide for themselves) and follow up the waiting times at the hospital emergency services and verify if the guaranteed response time for the waiting lists are being safeguarded. The platform also includes an area designated ‘Transparência’ (Transparency), with a set of information and indicators structured into four subareas – Access, Quality, Efficiency, Portuguese Health – with information related to the expenditure on medicines, number of mammograms performed in 2016 or how many vaccines were given in a specific heath centre. This information can be georeferenced and compared between different areas.
Regarding the professionals, this portal also represents an added value, allowing the access to the SNS software applications, the information about legislation and standards, checking orientations and guidelines and accessing to calls for tenders, training and events.
It should be also noted that in the other areas, namely ‘SNS’, it is possible to access information about user fees cross-border healthcare or simply to search for health centres, hospitals or pharmacies at national level. In the area ‘Institucional’(Institutional) there are the documents of reference such as the National Health Plan or the priority national health programmes at the Directorate General for Health. Finally, it is important to highlight that the ‘Portal do SNS’ (NHS web portal) allows access to an integrated set of indicators related to human, financial and institutional resources.
Another improvement in the SNS is the introduction of the electronic prescription of drugs, allowing the citizens to have all or part of the prescribed drugs dispensed in different pharmacies on the mainland and in the islands of Madeira and Azores.
The first results regarding the implementation of this mechanism are excellent. The first pilot experience of electronic prescription of drugs in the hospital environment was presented in the second quarter of 2015. At national level, by 15 November 2016, this system accounted for more than 99% of the total prescriptions in the public healthcare facilities and in the private sector exceeds 56%. Regarding the global results on the Regional Health Administrations (ARS), the five ARS account for more than 99% of the prescription of drugs, with exception of the ARS Centro (with 98,43%). In the private sector, the ARS Centro presented the highest percentage with 59%, followed by the ARS Lisboa e Vale do Tejo (58%), ARS Norte (54.46%), ARS Alentejo (52.86%) and ARS Algarve (51,76%). This system is now being implemented in the Islands of Madeira (the trial phase started in October 2016 and with 8% of practical results) (SPMS, 2016).
Another important innovation is the implementation in the SNS of the Free Circulation an Access (FAC) – Livre Acesso e Circulação (LAC) – which started in May 2016. This mechanism allows the user, jointly with the family physician (responsible for the patient referral), to choose any public hospital within the SNS where the speciality exists. The referral takes place according with the users’ needs in terms of geographical proximity and the average response times in each of the public hospital. The travel expenses are covered by the SNS if and when the user has duly proven the economic need for it and if/or the clinical condition justifies it in accordance with the defined criteria in the applicable legislation (MA.ACSS, 2016).
The FAC embodies a very important step for the improvement of access and equity, thus contributing to the progressive implementation of the SNS Integrated Access Management System – Sistema Integrado de Gestão do Acesso no SNS (SIGA SNS), which is one of the health priorities defined in the Programme of the 21st Constitutional Government.
The ‘SIGA_SNS’ and the FAC implementation represent an opportunity for the improving the user’s access with a global impact for SNS, hospitals, primary healthcare and in the response provided to the users’ needs. In the first six months of 2016, the FAC implementation in the SNS (between 1 June and 22 November) showed that 83.184 users were referred to a first appointment outside the usual hospital network (MS.ACSS, 2016).
Could you present us the two/three expectations that you have for 2017?
There are expectations regarding certain projects within the SNS. One of them refers to the recent implementation in public hospitals of the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10-CM/PCS) – that started on 1 January 2017. This codification system applies to all episodes for which the date of the first codification equals or surpasses 1 January 2017, regardless of the episode discharge date.
This changes from the ICD-9-CM to ICD-10-CM/PCS was mainly due to the limitations to properly reflect the diversity of diagnoses and procedures as well as the acknowledgement that the ICD-10-CM/PCS provides a more exhaustive and adequate methodology to mirror the nosological innovations. The ICD-10-CM/PCS provides a more updated clinical terminology, which is compatible with the present clinical practices when it comes to making the characterisation of morbidity. Moreover, it will allow the best conditions for the definition of more equitable financing models, therefore promoting the good practices and clinical innovation. The higher clinical specificity of ICD-10-CM/PCS represents a significant improvement in the hospital morbidity classification leading to the inclusion of higher details in the data codification (MS.ACSS, 2016).
Even though this new codification system will imply training to physicians and the adaptation of software, it represents an improvement in the quality and in the refinement of the information available to decision-makers and health managers. It also improves the hospital payment models consequently promoting the transparency, efficiency and effectiveness that we all want for the benefit of the healthcare system. This process will be closely monitored.
Another structuring project that will have our major focus and that was referred to in the previous paragraphs is regarding the new mechanism for accessing the healthcare in the Portuguese hospitals through the Free Circulation and Access (FAC) – Livre Acesso e Circulação (LAC).
It is imperative to create a shift in the healthcare demand paradigm by restructuring the system and making it about the patient and his needs and expectations, thus ensuring the equity when it comes to access, the quality of services and humanised, timely and sustainable healthcare services (MS.ACSS, 2016). In alignment with these premises we do expect the highest contributions from the FAC for the promotion of equity and a better and timely access to hospitals and healthcare as well as to the improvement of efficiency and effectiveness of hospitals and of the SNS.
The implementation of the FAC system presents numerous advantages for patients because it ensures them the opportunity of the free choice. The advantage for the professionals, especially the family physicians consists in improving the existing trust relationship that must exist with the patients while the one for the SNS consists in improving the efficiency, maximising the installed capacity and quality of healthcare services and ensuring the continuity of care to the users. However, this system could lead to some constrains regarding the users’ preferences for certain hospitals which in turn may lead to a substantial increase in the guaranteed response times by speciality. This will need a more detailed analysis and implementation time to understand the real impact of the FAC.
In the hospital sector, it is fundamental to introduce the Free Circulation and Access in the SNS (FAC). This area is of outmost importance for the operationalization of some of the measures defined by the hospital reforms which is in fact the main area of interest of the APDH. The Ministry of Health published the terms of reference for the contracting with public hospitals for 2017, including for the first time this area of FAC, among others relevant areas such as the implementation of the SNS Integrated Access Management System – Sistema Integrado de Gestão do Acesso no SNS (SIGA SNS) and assurance of the compliance of guaranteed response times.
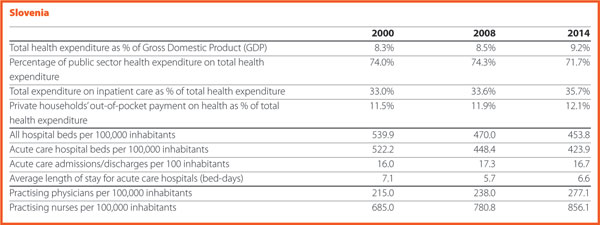
Slovenia

Simon Vrhunec HOPE Governor, Association of Health Institutions of Slovenia
Could you present the two/three main changes that happened in the hospital and healthcare sector in your country in 2016?
The economic situation in Slovenia improved during 2016. Consequently, it was expected that such improvement would have positively affected the healthcare sector especially the hospital sector. Several measures have been accepted since the beginning of the economic recession but during the year none of them has been implemented. This led to an increase of waiting times as well as disappointment of both patients and health workforce. In particular, more doctors claimed higher salaries during a strike at the end of the year. By contrast, the main positive change for hospital sector was that at the beginning of 2016 ten new hospital emergency centres were inaugurated and became functional. This represents one of the biggest investment in healthcare sector, mainly financed by EU funds.
Could you present us the two/three expectations that you have for 2017?
The expectations for 2017 regard the impact on the economic situation in the hospital sector. At the beginning of the year, many hospitals are facing liquidity problems, which are expected to be solved by the resources of the state budget. The salaries in public sector will continue to increase. Because the cost of the health workforce represents more than 60% of all costs, the expectation in relation to the hospital sector is that this increase will be covered through higher prices. Furthermore, since the waiting lists are increasing, the expectation is that financial resources will be transferred to decrease both waiting lists and waiting times. Finally, there is the expectation that the reform of the healthcare system on which the Ministry of Health is working now will improve the organisation and management of hospitals and other healthcare institutions and that it will provide an adequate financing of healthcare services.
Spain

Asunción Ruiz de la Sierra Head of Service, Ministry of Health, Social Services and Equality
Could you present the two/three main changes that happened in the hospital and healthcare sector in your country in 2016?
European Reference Networks (ERN)
In Spain, 42 Reference Centres, Services and Units (CSUR) have been designated to improve the provision of healthcare services. Moreover, these have been included in 17 ERN while the University Hospital La Paz has been appointed as the provider in charge of coordinating the Transchild ERN, dealing with transplants in children.
The project designating the Reference Centres, Services and Units (CSUR) of the Spanish National Health System (NHS) has the following objectives:
- Improving equity in access of all citizens to highly specialised services when needed;
- Concentrating the experience with a high level of specialisation ensuring high quality, safe and efficient healthcare;
- Improving care of low prevalence pathologies and procedures.
So far and subject to continuous updating, a total of 227 CSUR (concentrated in 46 centres) have been designated for the care or management of 52 pathologies or procedures.
The National Transplant Organization (ONT)
Spain is the world leader in terms of organ donations and transplants, accounting for 100.7 transplants and 43.4 donors per one million populations in 2016. According to the American Journal of Transplantation, “learning from the Spanish system would help solve the global problem of organ shortage for transplantation”.
Could you present us the two/three expectations that you have for 2017?
Quality Improvement Strategy of the Spanish Medical Societies: RECALCAR and others
The Spanish Society of Cardiology (SSC) recently launched a strategy for quality improvement in cardiovascular disease healthcare named SEC-CALIDAD (SSC-Quality). The RECALCAR (Resources & Quality in Cardiology) registry is a key element of this strategy.
The NHS of Spain is a public health care service agency that covers the whole population. The administrative organisation of Spain is based on 17 regions. This decentralised health care system model may produce inter-regional inequities in the quality of healthcare services. The Spanish Medical Societies are collaborating with the Ministry of Health to promote strategies that aim to improve and homogenise the quality of medical care in Spain, and to diminish these inequities. One of these strategies is the RECALCAR project. RECALCAR (Resources & Quality in Cardiology) started in 2012.
Investigating the association between health care outcomes and structure, resources, activity, and the management of hospitals and cardiac units is a basic pillar of RECALCAR. The registry has shown significant differences between Spanish regions and between hospitals in terms of healthcare quality, and in the management of acute myocardial infarction mortality and readmissions, which has led to organisational health care reforms. At this moment RECALCAR is analysing the association between heart failure management and health outcomes.
As a scientific society, the Spanish Society of Cardiology is seeking to systematically investigate the structure, resources, activity, and management of cardiac units with health care outcomes. RECALCAR deepens the focus of the US Centres for Medicare & Medicaid Services on the basis of hospital characteristics (mainly volume), attending also to specific arrangements for heart disease care in the hospital setting. RECALCAR Registry has been designated by the Ministry of Health as a ‘reference registry’ for the National Health System.
Following the path of the Spanish Society of Cardiology, other medical societies are developing RECAL (Resources & Quality) projects. The Spanish Society of Internal Medicine launched the project Resources and Quality in Internal Medicine (RECALMIN) in 2015, as the Spanish Society of Medical Oncology, Resources and Quality in Medical Oncology (RECALON). In 2016, the Spanish society of Digestive System and the Spanish Society of Pneumology started their respective RECAL projects. The Spanish Society of Endocrinology and Nutrition will launch its RECAL project in 2017 and there are other medical and surgical societies studying the development of RECAL projects.
Strategic plan for tackling hepatitis C in the Spanish National Health System
In view of the health problem posed by chronic hepatitis C in our country, the Spanish National Health System’s Interterritorial Council unanimously adopted a resolution at its meeting held on 14 January 2015 in favour of preparing a strategic plan for tackling hepatitis C in the Spanish National Health System. This Plan has been led by the Secretary General of Healthcare and Consumers Affairs of the Ministry of Health, Social Services and Equality.
This Plan is structured in four strategic directions, setting out some specific objectives and top-priority actions to be carried out over the course of the next three years (2015–2017), which will be carried out in collaboration with different agents: Regional Health Services, the Ministry of Health, Social Services and Equality, Management Centres, prison institutions and the Carlos III Health Institute.
New antiviral drugs have recently been launched on the market to fight hepatitis C. These are more effective, safer and better-tolerated than the former ones, making it possible to envisage a radical change in the current approach to tackling this disease. The use of direct-acting antivirals simplifies the treatment, considerably reduces the needs for monitoring, increases the cure rates for this infection and delays the onset of the later, severe complications of this disease. At the same time, we are currently lacking sufficient information on actual practice as to the therapeutic efficacy of these drugs and their effect in terms of health outcomes.
This Plan shall therefore put into practice measures including the assessment of the magnitude of this problem, access to the new drugs under actual conditions of equality and monitoring of their therapeutic efficacy. A systematic follow-up will be conducted, making it possible to assess the degree of implementation thereof and the outcomes achieved.
Sweden

Erik Svanfeldt HOPE Governor, Swedish Association of Local Authorities and Regions
Could you present the two/three main changes that happened in the hospital and healthcare sector in your country in 2016?
In Sweden, the county councils/regions are responsible for healthcare. The new Swedish minority government (Social Democrats and the Green Party), which took office in October 2014, wanted to implement a regional reform, establishing fewer and larger regions. One reason for this was to create economically stronger regional health authorities and facilitate structural changes in highly specialised healthcare. But the Government stopped the work on this reform when it became clear that a proposal for such changes of the regional structures would not have get enough support in the Swedish Parliament. In parallel, proposals have been put in government inquiries on how to make the Swedish healthcare more efficient by improving primary care services and concentrating highly specialised hospital care.
Could you present us the two/three expectations that you have for 2017?
In 2017, main topics on the political agenda will probably continue to be: coordination and concentration of highly specialised healthcare; equality in health and healthcare services; number of hospital beds; recruitment of doctors, nurses and other health professionals; further steps to improve healthcare by using digital technologies; profits made by private companies providing welfare services; long-term financing of healthcare.

United Kingdom

Elisabetta Zanon Director, NHS European Office
Could you present the two/three main changes that happened in the hospital and healthcare sector in your country in 2016?
A new strategic planning approach for the NHS
The Five Year Forward View is a wide-ranging strategy for the NHS in England that was published in October 2014 and which covers a number of themes, such as the importance of public health and ill-health prevention, empowering patients and communities, and making further efficiencies within the health service.
The strategy has identified the following key challenges for the NHS:
- the health and wellbeing gap – the urgent need to reduce demand on the NHS by shifting focus and investing in prevention services and addressing health inequalities
- the care and quality gap – reduce variations in the quality, safety and outcomes in care by greater use of technologies and innovations
- the funding and efficiency gap – to ensure the long term financial sustainability of the NHS and that additional funding is used to improve efficiencies and transform services.
The Five Year Forward View provides a vision for the NHS to deliver new models of care with a greater focus on prevention and integration, in order to address this triple challenge and improve outcomes for patients and communities.
A key means by which to achieve this objective is the development of Sustainability and Transformation Plans. In practice these Plans imply that, in different local areas, parts of the health and social care system will work together to provide more co-ordinated services to patients and to collectively manage the financial resources available for the services for their local population.
Forty-four areas have been identified across England as the geographical ‘footprints’ in which the plans are based, with an average population size of 1.2 million. The plans were submitted by the local areas in October 2016, with proposals put forward to improve health and wellbeing, quality of services and efficiency for the period until March 2021.
The geographical footprints were defined taking into account local communities, existing working relationships, patient flows and the scale needed to deliver the services, transformation and public health programmes. This approach represents a very new way of working for the NHS and has proved to be challenging, as the pressures facing local services are significant and the timescales for developing the plans have been extremely tight.
Sustainability and Transformation Plans provide an important opportunity for improving health and care services in England. Yet with the limited funding made available for this ambitious transformation programme, it remains to be seen to which extent they will be able to deliver new models of care on the ground.
Could you present us the two/three expectations that you have for 2017?
Possible implications of Brexit for the NHS
The NHS’s funding depends largely on the overall performance of the economy. A risk for the NHS arising from Brexit is therefore linked to a possible prolonged period of economic slowdown. Leading economists are almost unanimous in concluding that leaving the EU will have a negative effect on the UK economy, which in turn will impact on public spending. The impact of Brexit on the UK’s economy is however very difficult to quantify at the moment, as the situation will evolve constantly and hard data on the economy will not be available for some months.
The NHS is heavily reliant on EU workers, with around 10% of our doctors and 5% of our nurses being EU migrants. The biggest danger in the short term is that the prospect of Brexit could discourage EU citizens from staying or coming to the UK, due to fears of being unwelcome and concerns around employment rights. There is also speculation about the impact of a less favourable exchange rate, making the UK a less attractive destination for healthcare workers to live and work. In the longer term, everything will depend on the outcome of the negotiations between the EU and the UK and on which new immigration system the UK would put in place. The UK Prime Minister and Government have confirmed their intention to have a system, which enables migration to be reduced and better managed. There are different ways in which this could be achieved and it will be crucial for the NHS to actively seek to influence the new system in a positive way, while reducing its dependence from incoming professionals.
Brexit could also impact on NHS clinical research and innovation. Collaboration with leading counterparts across Europe has helped us to develop new treatments, adopt innovation more quickly, and improve the quality of healthcare we provide to our patients. It has also facilitated enrolment of NHS patients in clinical trials, allowing them to access innovative, life-saving treatments, when no other medical option was available to them.
The NHS’s participation in EU collaborative research will be impacted in the event the UK no longer had access to the EU framework programme for research post-Brexit, and were the UK’s regulatory framework (on clinical trials, authorisation of new medicines, data privacy, etc) to diverge from the EU’s in the future. Under this scenario, there could be implications in terms of patient care, (due to a potential slowing down of the take-up of innovations and their translation into NHS medical practice) and the NHS’s ability to attract and retain some of the most renowned clinicians in the world (who often decide to work for the NHS due to its reputation in leading medical research).