In England in 2013, there were 28,000 cases where emergency medical services (EMS) were called to attempt resuscitation for out of hospital cardiac arrest (OHCA).1 Other large studies give an incidence of OHCA of approximately 80 per 100,000 patient years.2 Worldwide, this figure is significantly higher than in Asia but falls slightly behind the USA and Australia.2 These numbers are only the amount of cases where EMS were called to OHCA, not how many were treated, or indeed how many had a cardiac cause, or
how many of those with cardiac cause were found to be in ventricular fibrillation (VF). This is important as there are positive survival rates associated with VF cases of OHCA versus any other.3
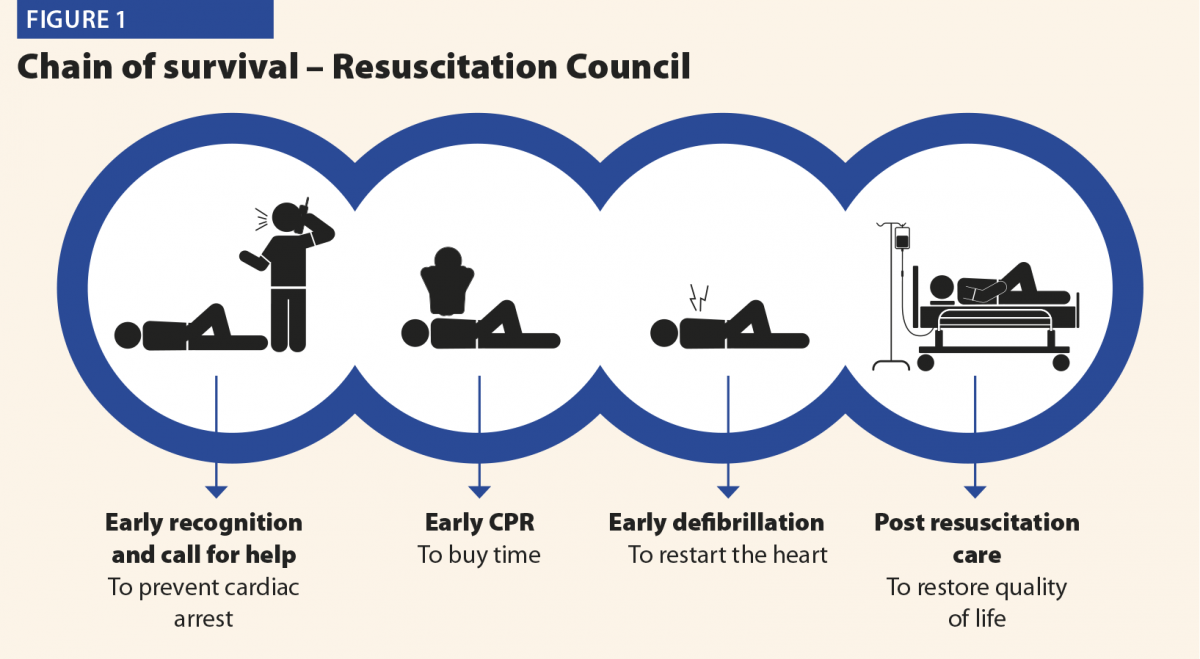
Mild therapeutic hypothermia (MTH), or targeted temperature management (TTM) as it is now more commonly known, has been established for the post-resuscitation care of OHCA since two pivotal studies in 2002.4,5 In the UK, it is incorporated into Resuscitation Council guidelines as the fourth link in the chain of survival (post-resuscitation care; Figure 1). This was supported by the International Liaison Committee on Resuscitation (ILCOR) in 2015.6
This review aims to look at the theory behind TTM and how it is applied clinically, with attention to new research in this field and what impact TTM has on patient survival and neurological recovery.
Previous work and history
Hippocrates and the Persian army had already commented on the protective nature of cold for centuries before Napoleon’s chief surgeon, Dominique Jean Larrey, documented that injured soldiers kept closer to the fire died more frequently than those kept away.7 Studies from the middle of the 20th century looked into MTH following both severe head injury and cardiac arrest,8,9 but the results were uncertain and not incorporated into standard practice.
Pivotal case reports exist of survival from acute hypothermia with intact neurology, possibly none more dramatic than that of Anna Bagenholm, trapped under the ice in Norway for 80 minutes after a skiing accident in 1999, and surviving to this day to work as a doctor. Her core temperature was recorded at 13.7°C on arrival at hospital, and her heart started after slow rewarming on cardiac bypass. It is only in the last 15–20 years that studies have progressed to looking not only at survival rates post-OHCA but also what degree of neurological deficit exists after TTM is instigated.
Mechanism of protection
Understanding that the damage to the brain occurs after cardiac arrest from hypoxia is paramount. There is no substitute for early recognition, early CPR and early defibrillation as laid out by the Resuscitation Council to reduce morbidity and mortality for OHCA. However once primary neurological insult has occurred, there should be every effort made to reduce the secondary reperfusion injury to the brain.
The mechanism of this injury is thought to be governed by free radical formation and inflammatory mediators such as TNFα and interleukin-1.10 During this ischaemia–reperfusion time, it is suspected that ATP molecules are reduced in the brain and anaerobic glycolysis occurs, causing intracellular levels of phosphate, hydrogen and lactate to rise; this, in turn, leads to intra- and extracellular acidosis and subsequently cell apoptosis and death.10
It is known in animals that there is reduction in cerebral metabolic rate for oxygen (CMRO2) of 6% for every 1-degree reduction in brain temperature (>28°).11 It is theorised that the injured brain could be therefore be protected in this critical post-resuscitation period. There is also evidence that a 4–5-fold increase in oxygen radicals may be present in hyperthermia.12 Subsequently this is suggested to be a factor in why hyperthermic patients suffering OHCA have an increased mortality rate and incidence of neurological sequlae.13
Complications
While inducing hypothermia for TTM seems to convey protection, it is not without risk. The documented side effects for this treatment range from diuresis causing electrolyte disturbance, shivering (causing need for muscle relaxation, thus masking seizure activity) to cardiac dysrhythmia, bleeding and immune suppression. A review listed cardiovascular complications as the most likely to occur, but deemed this due to pre-existing ischaemic heart disease (IHD) exacerbated by the haemodynamic imbalance caused by TTM.14
One key area of complication with TTM is glucose homeostasis, specifically with insulin resistance and reduced insulin secretion leading to hyperglycaemia; this causes an increase in the rate of infections, neuropathy and renal failure. Overall morbidity and mortality has been shown to be higher with hyperglycaemia in the critically ill population and therefore close monitoring and appropriate management of hyperglycaemia should be undertaken with TTM.14 In our hospital, we use a concentrated dextrose infusion with variable rate insulin regime to control blood glucose levels within a targeted range.
Techniques
The reason TTM has replaced MTH or TH is to place the importance on defining a temperature profile for a patient, manipulating their physiological response.15 It can be divided into three phases:
- Induction – an intentional change from current temperature to a lower one
- Maintenance – maintaining the set temperature for a desired time
- Rewarming – changing to a new normothermic temperature value by increasing temperature at a set rate.
Research exists on the optimal time to instigate TTM, its length of duration and rewarming time, with some studies even performing pre-hospital MTH, unfortunately without benefit to long-term survival or disability.16
All early studies seemed to conclude that TTM should be started as early as is feasibly possible; however, a randomised, controlled trial did not prove any benefit in terms of speed to achieve MTH in comparison to TTM and avoidance of hyperthermia.17
There are currently three main techniques available for cooling post-OHCA. These are summarised below, and the availability of each varies depending on location and on financial circumstances:
- Conventional cooling methods
- Surface cooling systems
- Intravascular cooling systems.
Conventional cooling methods
These methods include crushed ice, ice bags and the infusion of cold fluid. These have the advantage of being cheap, mostly accessible, and can be used in combination with other methods. These methods however are somewhat crude, and while an evidence base for adequately lowering temperature is available,18 they can reduce temperature to undesired levels and be difficult
to use in maintenance of desired temperature range.
Surface cooling methods
These devices, probably the most commonly available, work by circulating cold fluid or air through either blankets or pads wrapped or applied to the patient. A number of devices exist: blankets such as the Curewrap with CritCool by MTRE, and Kool-Kit with Blanketrol III by Cincinnati Sub-Zero are popular. The InnerCool STX by Philips and Arctic Sun by Medivance are examples of pad devices, the latter currently being used in our hospital.
The advantages of these devices are that they are easy to apply and rapidly initiate treatment, while also offering auto-feedback mechanisms to adjust water or air temperature accordingly in keeping with patient assessment from skin and core temperature sensors.
Unfortunately shivering is most common with these devices,19 which might necessitate muscle relaxation. There is also the possibility of skin irritation and burns, although these are rare.19
Intravascular cooling methods
These methods involve the cannulation of a central vein which comes with its own risks and complications, namely infection, bleeding and thrombosis. At time of writing, the Thermoguard XP (Zoll) and InnerCool RTx (Philips) are the major devices in use. The Thermoguard has the added benefit of having a triple lumen infusion catheter combined with its cooling system avoiding the need for multiple lines. The greatest benefit ascertained with these devices is precise temperature control in maintenance and rewarming phases and less shivering.20
Comparison of cooling methods
Conventional methods aside, a recent retrospective study looked at surface cooling methods versus intravascular cooling devices.21 The analysis identified there was no change in outcome in either mortality or neurological deficit between these two methods. Statistically there were significantly more patients out of temperature range while maintaining therapy in the surface cooling group, and an increase in median time spent outside targeted temperature as well. This work further supported earlier studies22 that advocated the use of either surface pads or intravascular devices for the induction of hypothermia but strongly recommended intravascular devices for maintaining target temperature.
The National Institute for Health and Care Excellence updated its advice on TTM in July 2017 to advocate the use of Arctic Sun over conventional or intravascular cooling methods, due to a combination of reduced risks associated and the potential for improved outcomes.
Conclusions
TTM is an extensively researched, effective, neuroprotective strategy with well established guidelines; however, confusion exists about the optimal duration and target temperature. At the time of writing, the most up-to date research would advocate starting TTM as soon as feasibly possible, but not setting low temperatures (that is, 33°C) and simply avoiding temperatures above 36°C.17 This obviously remains at the clinician’s discretion and temperatures between 35 and 36°C are commonplace.
While new devices and research into this treatment are evolving and being undertaken, it is important to reflect on the fundamentals. First, patient selection remains an often-overlooked area, and the authors urge vigilance in selecting those patients who are suitable for instigation of TTM and screening carefully for those likely to benefit from this therapy. To this point, if there is doubt regarding the initial rhythm of arrest, then TTM should be instigated and not withheld.
The clinician involved in the decision to commence TTM must pay attention to the precise control of temperature in all phases, and critically in the rewarming phase where a passive, non-controlled rise could have serious effects on outcome.
Finally, as with most evolving medical research, there is more work to be done, particularly now that 36°C temperatures are associated with equal outcomes to 33°C. Are we ready to accept normothermia and adopt cooling measures when we see a trend to hyperthermia?
References
1 London Ambulance Service Cardiac Arrest Annual Report 2012/2013. www.londonambulance.nhs.uk.
2 Berdowski J et al. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 2010;81(11):1479–87.
3 Perkins GD, Brace-McDonnell SJ. The UK Out of Hospital Cardiac Arrest Outcome (OHCAO) project. BMJ Open 2015;5(10):e008736.
4 Bernard SA et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 2002;346(8):557–63.
5 The Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 2002;346(8):549–56.
6 Monsieurs KG et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 1. Executive summary. Resuscitation 2015;95:1–80.
7 Gajić V. [Forgotten great men of medicine – Baron Dominique Jean Larrey (1766-1842)]. Med Pregl 2011;64(1–2):97–100.
8 Benson DW et al. The use of hypothermia after cardiac arrest. Anesth Analg 1959;38:423–8.
9 Williams GR, Spencer FC. The clinical use of hypothermia following cardiac arrest. Ann Surg 1958;148(3):462–8.
10 Knot J, Moťovská Z. Therapeutic hypothermia after cardiac arrest – Part 1: Mechanism of action, techniques of cooling, and adverse events. Cor et Vasa 2012;54(4):e237–42.
11 Steen PA et al. Hypothermia and barbiturates: individual and combined effects on canine cerebral oxygen consumption. Anesthesiology 1983;58(6):527–32.
12 Globus MY-T et al. Detection of free radical activity during transient global ischemia and recirculation: Effects of intraischemic brain temperature modulation. J Neurochem 1995;65(3):1250–6.
13 Zeiner A et al. Hyperthermia after cardiac arrest is associated with an unfavorable neurologic outcome. Arch Int Med 2001;161(16):2007–12.
14 Soleimanpour H et al. Main complications of mild induced hypothermia after cardiac arrest: A review article. J Cardiovasc Thorac Res. 2014;6(1):1–8.
15 Vaity C, Al-Subaie N, Cecconi M. Cooling techniques for targeted temperature management post-cardiac arrest. Crit Care [Internet]. 2015 [cited 2017 Nov 21];19(1). www.ncbi.nlm.nih.gov/pmc/articles/PMC4361155/ (accessed July 2018).
16 Diao M et al. Prehospital therapeutic hypothermia after cardiac arrest: A systematic review and meta-analysis of randomized controlled trials. Resuscitation 2013;84(8):1021–8.
17 Nielsen N et al. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med 2013;369(23):2197–206.
18 Larsson I-M, Wallin E, Rubertsson S. Cold saline infusion and ice packs alone are effective in inducing and maintaining therapeutic hypothermia after cardiac arrest. Resuscitation 2010;81(1):15–19.
19 Mayer SA et al. Clinical trial of a novel surface cooling system for fever control in neurocritical care patients. Crit Care Med 2004;32(12):2508–15.
20 Lyden PD et al. Intravascular cooling in the treatment of stroke (ICTuS): early clinical experience. J Stroke Cerebrovasc Dis 2005;14(3):107–14.
21 Glover GW et al. Intravascular versus surface cooling for targeted temperature management after out-of-hospital cardiac arrest – an analysis of the TTM trial data. Crit Care 2016;20(1):381.
22 Hoedemaekers CW et al. Comparison of cooling methods to induce and maintain normo- and hypothermia in intensive care unit patients: a prospective intervention study. Crit Care 2007;11(4):R91.