Basilea Pharmaceutica AG announces the UK launch of its broad-spectrum Cephalosporin Zevtera® (Ceftobiprole medocaril) for the first-line treatment of serious bacterial pneumonia.
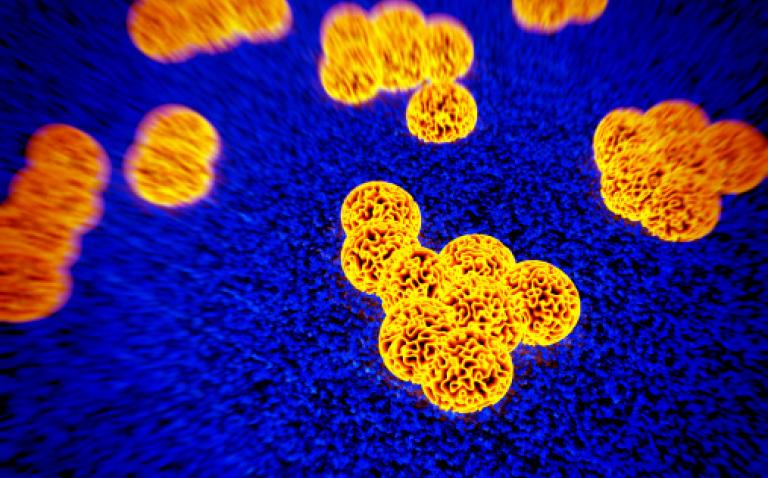
Zevtera® is the only antibiotic approved as a monotherapy in the UK for the treatment of community-acquired (CAP) and hospital-acquired (nosocomial) pneumonia (HAP) (excluding ventilator-associated pneumonia (VAP)), that is effective against Methicillin-resistant Staphylococcus aureus (MRSA) and gram-negative pathogens such as strains of Pseudomonas aeruginosa and Enterobacteriaceae. (1)
The emergence of resistant strains of bacteria has been described by the World Health Organisation (WHO) as the single greatest challenge in infectious diseases today. (2) According to a UK review on antimicrobial resistance (AMR), by 2050 the global cost of AMR will be up to $100 trillion and will account for 10 million extra deaths a year. (2) The UK and the international community have made a commitment to tackle AMR with key areas of focus including rapid diagnostics and new drug development in order to sustain the supply of effective treatments available in the future. (2) Zevtera® is a new therapy option for clinicians in the UK, with its fast-acting bactericidal activity against a large variety of gram-positive and gram-negative pathogens. In particular it is effective against resistant pathogens such as MRSA or Penicillin- and Ceftriaxone-resistant pneumococci. (3,4) Zevtera® is indicated for the treatment of CAP and HAP, which are common and lead to a high mortality rate in the UK. (5)
Simple administration as monotherapy
Zevtera® contains Ceftobiprole, the active ingredient of the water-soluble prodrug Ceftobiprole medocaril. The active ingredient belongs to the latest generation of Cephalosporin* antibiotics. (3)
Zevtera® is administered intravenously as a monotherapy, can be used as empiric therapy, and is based on a dose of 500mg once every eight hours. (1) It demonstrates predictable and linear pharmacokinetic properties. It is excreted largely unchanged via the kidneys and therefore no dose adjustments are required for patients with impaired liver function. Also the risk of clinically relevant interaction with other simultaneously administered medication is low. (1)
Efficacy demonstrated in two Phase III trials
The efficacy and tolerability of Zevtera® has been demonstrated in two Phase III trials relevant to its licencing for use in patients with CAP and HAP. In an international, double blind, randomised trial with 781 patients with HAP the non-inferiority of Zevtera® compared to Ceftazidime plus Linezolid was demonstrated. The clinical cure at the test-of-cure visit 7–14 days after the end of the therapy (primary endpoint) was achieved by 69.3% with Zevtera® and 71.3% with the combination. (6) Non-inferiority of Zevtera® versus the comparator therapy could not be demonstrated for VAP.
In a further multicentre, double blind, randomised study Zevtera® had non-inferior efficacy in 638 hospitalised patients with CAP compared to Ceftriaxone with or without Linezolid. The primary endpoint, clinical cure at the test-of-cure visit 7–14 days after the end of the therapy, was achieved by 86.6% receiving Zevtera® therapy and by 87.4% of patients in the group receiving Ceftriaxone with or without Linezolid. The non-inferiority of Zevtera® was also demonstrated with the intent-to-treat (ITT) analysis. (7)
Post-hoc-analyses of the Phase III trial data show an early clinical response for Zevtera® particularly for HAP (with the exception of VAP) when compared to a standard combination of antibiotics. Zevtera® led as early as day four to a clinical cure or an improvement of the symptoms in 87% of patients (versus 78% for the comparator combination). The early improvement was particularly noticeable in patients with confirmed MRSA at baseline. 95% (versus 53% on the combination) of the MRSA-patients showed a clinical cure or improvement by day four. (7)
Ceftobiprole was well tolerated in clinical trials. The most frequent side effects in ≥3 % of patients treated with Zevtera® were nausea, vomiting, diarrhoea, reaction at the infusion site, hypersensitivity (including urticaria, itchy skin rash and drug allergy) and taste impairment. (1)
Extension of the infusion time with increased clearance
Renal function is frequently altered in patients in intensive care.
Increased renal clearance above the normal range may necessitate a change in infusion time. Data from a randomised parallel-group trial using Zevtera® was presented recently at the 25th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) in Copenhagen, Denmark. The trial of 33 intensive care patients, showed that a dose of 1000mg every 8 or 12 hours administered as an infusion over four hours was tolerated well by the patients. By doubling the infusion time in patients with a creatinine clearance >150ml/min the plasma levels could be maintained at above 4mg/ml. The authors of the research therefore recommend that patients with increased renal clearance receive an extended duration of infusion of Zevtera®. (8) This same recommendation is also included in the summary of product characteristics for Zevtera at the approved 500mg dose. (1)
A further post-hoc analysis of the Phase III data by Awad et al., presented at ECCMID 2015, showed that the bacterial profile of the patients with early or late onset HAP was similar and that the time to onset of HAP was not a strong predictor of the pathogen distribution. Zevtera® was similarly effective to Ceftazidime plus Linezolid both in early and in late onset HAP. (9)
References:
- Zevtera®. Summary of Product Characteristics. Available at: https://www.medicines.org.uk/emc/medicine/29764. Last accessed May 2015.
- Securing new drugs for future generations: the antibiotics pipeline. The review on antimicrobial resistance. Chaired by Jim O’Neill. Available at: http://amr-review.org/sites/default/files/SECURING%20NEW%20DRUGS%20FOR%20FUTURE%20GENERATIONS%20FINAL%20WEB_0.pdf. Last accessed May 2015.
- Bodmann KF, Grabein B, expert committee of the Paul-Ehrlich-Association for chemotherapy. Recommendations for empiric parenteral initial antibiotic therapy of bacterial diseases in adults: Update 2010. GMS Infectious Diseases. 2014; 2:Doc05. Available at: http://www.egms.de/static/en/journals/id/2014-2/id000013.shtml. Last accessed May 2015.
- Syed YY. Ceftobiprole medocaril: a review of its use in patients with hospital- or community-acquired pneumonia. Drugs 2014;74:1523–42.
- Pneumonia: Diagnosis and management of community- and hospital-acquired pneumonia in adults, NICE Clinical Guideline. December 2014. Available at: http://www.nice.org.uk/guidance/cg191/chapter/introduction. Last accessed May 2015.
- Awad SS et al. A phase 3 randomised double-blind comparison of ceftobiprole medocaril versus ceftazidime plus linezolid for the treatment of hospital-acquired pneumonia. Clin Infect Dis 2014;59:51–61.
- Nicholson SC et al. A randomised, double-blind trial comparing ceftobiprole medocaril with ceftriaxone with or without linezolid for the treatment of patients with community-acquired pneumonia requiring hospitalisation.Int J Antimicrob Agents 2012;39:240–6.
- Torres A et al. Pharmacokinetics, safety and tolerability of high-dose ceftobiprole medocaril administered as prolonged infusion in intensive-care-unit (ICU) patients. ECCMID. 2015;Kopenhagen:O199. Available at: http://eccmid.meetingexpert.net/ECCMID_546/poster_122537/program.aspx/anchor122537. Last accessed May 2015.
- Scheeren TW et al. Clinical cure and mortality outcomes with ceftobiprole medocaril versus ceftazidime plus linezolid in patients with early- versus late-onset hospital-acquired pneumonia. ECCMID. 2015:O194. Available at: http://eccmid.meetingexpert.net/ECCMID_546/poster_122532/program.aspx/anchor122532. Last accessed May 2015.
- Pneumonia. Patient.co.uk. Available at: http://www.patient.co.uk/doctor/pneumonia-pro. Last accessed May 2015.