A new study from the Center for Immunology and Inflammatory Diseases (CIID) at Massachusetts General Hospital (MGH) describes a method of reprogramming the regulatory T cells that usually suppress immune responses into inflammatory cells that not only permit but also intensify an antitumour immune response.1
“Many patients’ tumours do not respond to immune therapies – such as immune checkpoint blockade – because of a lack of pre-existing inflammation that is required for those therapies to work,” says Thorsten Mempel, MD, PhD, of the MGH CIID, senior author of the paper. “Our study shows that reprogrammed Treg cells provide exactly the type of inflammation that is lacking. Indeed, we found in mice that reprogramming tumour-infiltrating Treg cells to secrete inflammatory cytokines makes previously unresponsive tumours highly sensitive to PD-1 blockade.”
The study focused on the CBM complex – a large protein cluster within immune cells that helps regulate their activation, proliferation and function. Recent research has revealed a critical role for the CBM complex in lymphocyte function, and since deleting one of three key proteins, called CARMA1, is already known to reduce the function of effector T cells, the team examined the effects of CARMA1 deletion on Treg cells.
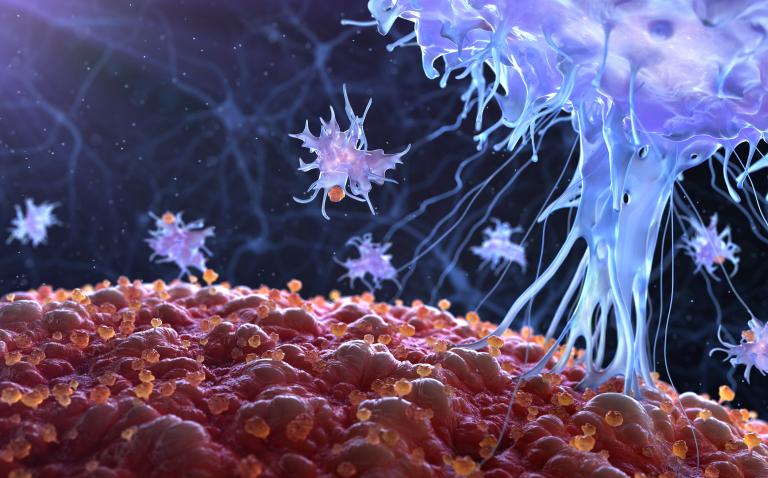
Their experiments revealed that targeting the CBM complex – either by deleting one or both copies of the CARMA1 gene in Treg cells or by treating tumour-bearing mice with a drug that inhibits MALT1, another component of the complex – caused Treg cells to secrete the immunostimulatory cytokine interferon gamma in tumour tissue alone. The ability to selectively modulate the function of Treg in tumours can avoid the risk of autoimmune disease that would result from systemic Treg depletion.
CBM targeting led to inflammation of tumour tissue and increased infiltration by cytotoxic CD8 T cells and natural killer cells. But it only reduced the rate of tumour growth in mouse models of melanoma and colon cancer because the activity of those immune cells was still limited by the immune checkpoint protein PD-1. However, blocking the activity of PD-1 with antibodies led to elimination of tumours that had been inflamed by anti-CBM treatment.
Reference
- Di Pilato M et al. Targeting the CBM complex causes Treg cells to prime tumours for immune checkpoint therapy. Nature 2019; DOI: 10.1038/s41586-019-1215-2