Breakthroughs in science and technology are creating exciting opportunities in healthcare planning and facility development. Physical barriers are falling; our health and social care are on course to extend across multiple environments. Whereas hospitals used to be the centres of healthcare, planners now need to consider a wider and more complex system.
The healthcare tech revolution
Everyone involved in planning healthcare systems will be aware of the speed and scale of technological developments that are upon us. Advancements in genomics and artificial intelligence, medical technologies and informatics, fuelled by big data, are empowering transformation in medicine, imaging, surgery and pharmacology, bringing us into the age of precision medicine.
Healthcare’s increasing virtual dimension means that future delivery will rely on integration, which will in turn demand further technological advances.
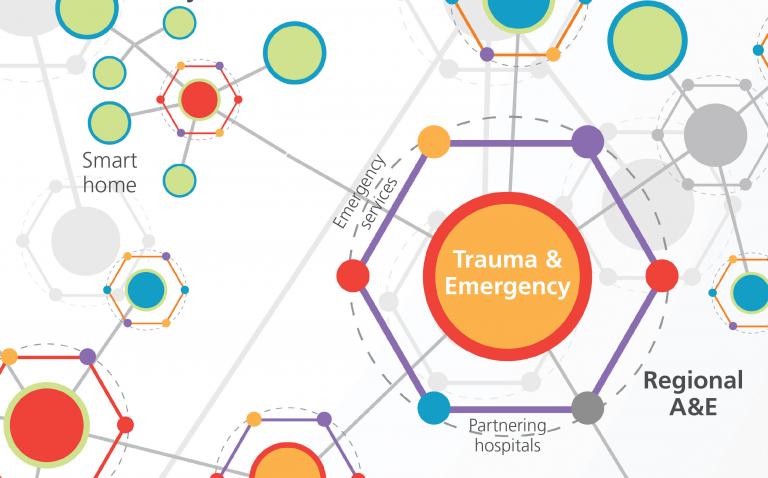
There are currently two streams of integration. One is developing across organisations and healthcare services. The other is integrating health and care facilities across the healthy city, the healthy home and the workplace. When these streams mature and merge, we will have created a holistic “healing machine”. This will help improve prevention, encouraging greater personal empowerment, as well as improving management of long-term conditions, to reduce emergency visits and unplanned admissions.
What will be the impact on hospitals?
To some this may appear to be a vision of de-hospitalisation. However, improved longevity alongside increased numbers living with complex conditions add to the burden of critical and specialist care. To us, it is apparent that health systems are under pressure to evolve, to develop new types of facilities, to expand their penetration into community settings, and to centralise highly specialist services, by taking advantage of new forms of healthcare integration.
The system will require a wider range of facilities than we see at present. And they will need to be resilient and highly responsive to change. Certain activities will need to be more centralised, others will be released to community settings. In some cases, centralisation will be via virtual integration, in others, highly specialist practitioners and their equipment will need to come together in specialist hospital settings.
In the future, clinicians will work in new ways, and the way patients relate to clinicians and to healthcare settings will be transformed.
Essentia is currently providing healthcare planning advice to a world-class, highly specialised hospital in South London. The vision for this hospital is to become a specialist care hub, fully integrated into a local, regional and national system with strong international partnerships and collaborations. It will need to be at the epicentre of its field of medical science.
Similarly, we are contributing to plans for a specialist hospital in Dubai closely associated with the project in South London. Clinical services will enjoy the benefits of integration between clinical teams in London and Dubai. Staff will in some cases travel between the sites, and patients too if necessary, but much will be done remotely via both new, and not-so-new technologies already available.
These are hospitals that will provide vital elements of the future healing machine. Neither will be self-sufficient, for the service will span vast geographies, will connect home to local care provider to specialist hospital, and will rely on shared information and expertise.
What benefits can we expect to see for patients and clinicians?
We can expect to see:
- Expertise anywhere, at any time
- Signposting – navigating the system to be in the right place, at the right time
- Faster bench-to-bedside translation in research
- Robotics for logistical support and other repetitive tasks
- Greater safety and precision in prescribing individualised medications, and emphasis on evidence-based care
- Care closer to home – and at home
- Remote care, remote surgery
- Remote ICU telemetry management and clinical advisory services
- Sharing of expertise across networks of mutually supporting collaborators
- Timesaving devices giving clinicians with more time with their patients
- Governance benefits from increasing integration of data platforms
- Improved flow management
- Improved care co-ordination
These in turn will offer opportunities for health and care providers to offer more personalised care, driven in part by consumer demand.
What hurdles do we need to overcome first?
Healthcare systems, such as the NHS in the UK, are already encouraging vertical and horizontal integration, and progression towards an integrated care model.
To achieve this, and to create new facilities to support this vision, hospital directors and planners will need to prioritise:
- Building resilience across the system such that hub capacity is maintained through effective management of patients’ care post the acute phase
- Ensuring that design solutions allow the new model of care to develop unimpeded, adapting over time, and supporting ground-breaking innovation that will free hospitals from the constraints of siloed care provision
- Avoiding stranded capacity in other hospitals and facilities within the healthcare system
- Harnessing technology to deliver more humane, personalised and thoughtful care – the gift of time – not merely short-term (and sometimes short-lived) efficiencies
- Using simulation tools to understand periodicity and peaking in demand and matching capacity accordingly
- Planning for the progressive retirement of existing models of care as system-wide initiatives alter demand pattern.
These changing flows of people, materials and information in healthcare will result in new project priorities and guiding principles.
What does this mean for healthcare planning and design?
Planners must work together alongside designers to develop the facilities that work for this new reality. New technologies will permeate every process and procedure in healthcare. Facilities and technology can no longer afford to be segregated.
There are lessons to be learned from several decades of experiments in health facility future-proofing strategies, but in other ways, we are in uncharted territories. As healthcare embraces new partners and new settings for care, planners and designers need to devise strategies for change that, with robust master planning, will stand the test of time.
The ability to replace physical with virtual flows or adjacencies, alongside system integration, will fundamentally change the way that spaces are used. Will the new ‘machine that heals’ help people and populations to achieve the best possible social, mental and physical wellbeing? That is up to all of us who play a part in healthcare delivery.
For more information on how Essentia can help with healthcare transformation projects, visit: www.essentia.uk.com