An eight-year hunt for the cells that drive the extreme childhood food allergy eosinophilic esophagitis (EoE) has identified a potential new way to treat the disease while also raising questions about a dietary supplement often taken to reduce bowel inflammation.
The study, led by experts at Cincinnati Children’s Hospital Medical Center, is posted online in the Journal of Clinical Investigation1 and will be published in print in May.
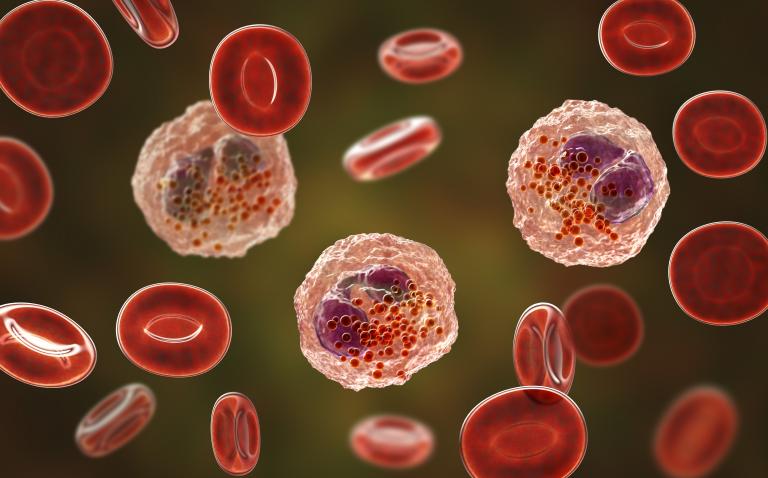
Reported cases of EoE have risen sharply in the past two decades, now affecting as many as one of every 2000 people. This lifelong allergic disease occurs when too many eosinophils cause inflammation that makes swallowing and eating painful. EoE can be so serious that some people depend upon special liquid formulas to eat.
In this study, Wen and Rothenberg developed and perfected a 10- to 12-hour process that isolates and analyses individual living cells from human tissue samples about the size of three sesame seeds.
“This is actually a substantial advance for the field,” Rothenberg says. “Prior work has focused on blood cells, but not the specific memory immune cells in tissue that directly respond to food allergens. We uncovered the unknown properties of these cells.”
Their key findings:
- Eight types of immune system T cells were found in the oesophageal tissue. That’s more than had been previously expected.
- Two cell types (T7 and T8) show up in higher numbers in the diseased tissue. The study finds that one of these two cell types responds to allergens by cranking out massive amounts of inflammation-causing type 2 cytokines.
- One of these cell types (T8) is nearly non-existent in healthy tissue, making it especially worth targeting for treatment. “These cells are bad actors that should not be in this type of tissue. Inhibiting these cells is now a central goal of our research,” Wen says.
- So how did these bad players get there? Studying this question led the co-authors to a surprising finding. One of the overactive genes that helps trigger the inflammation response – a gene called FFAR3 – also encodes a receptor for the dietary supplement butyrate.
Beyond EoE, the process used in this study could be applied in other, more-common conditions to find small populations of cellular culprits hiding within tissues. The study co-authors say the process could be useful in studying asthma, atopic dermatitis, allergic rhinitis, and other diseases associated with type 2 cytokines.
Reference
- Wen T et al. Single-cell RNA sequencing identifies inflammatory tissue T cells in eosinophilic esophagitis. J Clin Invest 2019;DOI: 10.1172/JCI125917