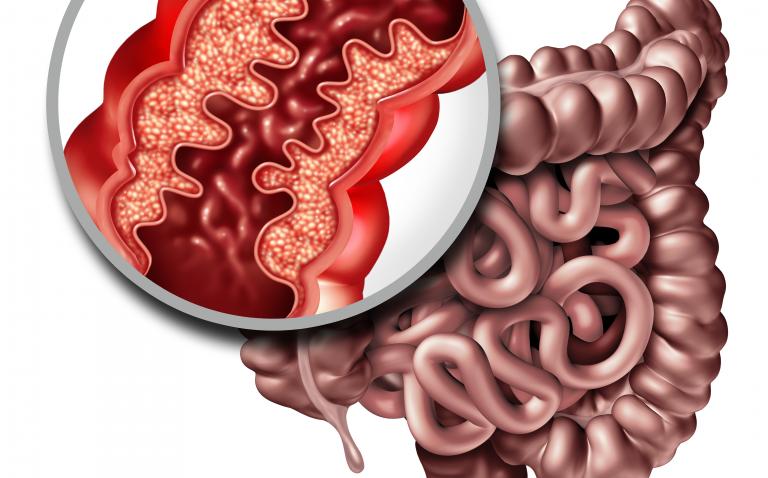
The diagnosis of Crohn’s disease (CD) does not rely on a single gold standard but requires the integration of clinical data with endoscopic, histologic, radiological and biochemical investigations.1
Biomarkers have become essential to discriminate CD from ulcerative colitis (UC), to grade the severity of inflammation because symptoms based scores are subjective, to measure the response to pharmacological options, to predict the risk of relapse and to monitor for postoperative recurrence.2
While erythrocyte sedimentation rate should be abandoned because of its low specificity, being also affected by haematocrit and physiological states such as pregnancy and age, C-reactive protein and faecal calprotectin (FC) are now widely used.
CRP is produced by hepatocytes in response to proinflammatory cytokines, chiefly interleukin-6 (IL-6), tumour necrosis factor alpha (TNF-alpha) and IL-1beta, and has a short half-life of about 19 hours, making it a more responsive indicator of acute inflammation. Meta-analyses have shown its role in the differential diagnosis between IBD and IBS and the correlation with endoscopic findings; however, specificity is low and about 25% of patients with active CD on endoscopy do not express levels of CRP above the normal threshold because of genetic variants.
FC is a neutrophil-derived protein excreted in the faeces and is a more reliable surrogate marker of inflammation, with a significant correlation with endoscopy. FC predicts mucosal healing and response to anti-TNF therapy, and has a prognostic role for disease course, even in the postoperative setting.3 There are, however, potential barriers in implementing its use in clinical practice as compared with CRP: patients’ dis-inclination to collect stools, lack of specificity as opposed to other infectious or inflammatory processes of the gut, different accuracy according to disease type (CD vs UC) and location (colitis vs enteritis), need for standardisation due to variability among different assays, and different cutoff thresholds depending upon the clinical scenario.
STRIDE vs CALM
Although the recommendations of the STRIDE consensus4 do not recognise biomarkers as a target for therapies, considering them as adjunctive measures for inflammation, the CALM study,5 which compares two different strategies in the management of CD with adalimumab, suggests a revision of these guidelines by incorporating FC as a treatment target. This study analyses treatment outcomes in two different groups, the first adopting a conventional strategy using only clinical criteria to guide escalation of therapy; the other, the tight control group, adopting biomarkers and especially FC to drive treatment optimisation. The tight control group had a significantly improved outcome. Self-monitoring at home of FC by a rapid test and the use of dedicated smartphones opens the door to a new way of monitoring the patients through telemedicine.6
Blood tests are recommended to select candidates to anti-TNFs (screening tests looking for HBV and HCV status and latent tuberculosis), to assess the risk of adverse events (testing for thiopurine metabolites and thiopurine-methyltransferase activity) and to personalise and optimise biologic therapy (therapeutic drug monitoring (TDM)).7 TDM measures drug levels and anti-drug antibodies and may allow identification of patients for whom dose escalation or intensification is warranted and patients for whom a therapeutic switch within the class or out of class is necessary, thus leading to a more appropriate and cost-effective management strategy of loss of response, which can involve from 13% to 20% of patients per year.
Pharmacogenetics, although presently confined to the assessment of thiopurine S-methyltransferase polymorphisms and haematological toxicity associated with thiopurine treatment, is a promising field that will contribute to a better understanding of the molecular mechanisms of variability in response to the drugs. Future perspectives will be the integration of the ‘omics’ in patients’ profiling to expand personalised care and precision medicine strategies in CD.8
References
- Gomollón F et al. 3rd European Evidence-based consensus on the diagnosis and management of Crohn’s Disease 2016: Part 1: Diagnosis and medical management. J Crohn’s Colitis 2017:3–25.
- Cappello M, Morreale GM. The role of laboratory tests in Crohn’s disease. Clin Med Insights: Gastroenterology 2016;951–62.
- Reenaers C et al. Expert opinion for use of faecal calprotectin in diagnosis and monitoring of inflammatory bowel disease in daily clinical practice. UEG J 2018;0(0) 1–9.
- Peyrin-Biroulet L et al. Selecting therapeutic targets in inflammatory bowel dDisease (STRIDE): Determining therapeutic goals for treat-to-target. Am J Gastroenterol 2015;110:1324–38.
- Colombel JF et al. Effect of tight control management on Crohn’s disease (CALM): a multicentre, randomised, controlled phase 3 trial. Lancet 2017;390:2779–89.
- Vinding KK et al. Fecal calprotectin measured by patients at home using smartphones—A new clinical tool in monitoring patients with inflammatory bowel disease. Inflamm Bowel Dis 2016;22:336–44.
- Vande Casteele N et al.Trough concentrations of infliximab guide dosing for patients with inflammatory bowel disease. Gastroenterology 2015;148:1320–9.
- Fiocchi C. Integrating Omics: The future of IBD? Dig Dis 2014;32(suppl 1):96–102.