The ubiquity of the pink ribbon campaign, the prevalence of precision medicine as a recurring theme in every scientific and medical journal, and the very fact that BRCA has entered the lexicon of society – globally – suggests that breast cancer testing is standard. Indeed, something that has been part of everyday life for some time.
Here, we will take a retrospective look at BRCA testing, highlight where breast cancer screening is today and the impact it is having on treatment decisions and look forward to the potential future of breast cancer screening.
BRCA testing – a retrospective
In 1990, Dr. Mary-Claire King, a luminary in science, published the paper that started the BRCA revolution.1 As the first to apply linkage analysis to demonstrate the association of a gene with a complex trait (a factor that would become critical to next generation sequencing (NGS) more than 20 years later), her lab identified the connection between familial / inherited breast cancer and a gene mapped to chromosome 17q21. The race to isolate and sequence the gene was on.
A few years later, King’s lab confirmed the germline association in a familial study,2 however, Mark Skolnick together with Myriad Genetics and McGill University announced that they had won the race by sequencing the gene and renaming it “BRCA1”.3 A year later, BRCA2 had also been sequenced.4
Myriad went on to patent BRCA1/2 which ignited intense controversy, enormous dissent around the $4,000 two-gene diagnostic screen and extensive litigation through to 2013 when the Supreme Court invalidated their patents unanimously ruling that “a naturally occurring DNA segment is a product of nature and not patent eligible merely because it has been isolated“.
The genetics of cancer is complicated and unpredictable. The rapid adoption of BRCA was surprising given the limited understanding of its molecular function and clinical effects. In 1996, Ruth Hubbard sounded the alarm on the pitfalls of genetic testing, specifically calling out the utility of the BRCA1 testing given that multiple variants of unknown health implications had been detected in the gene and that there were no known preventative measures – what should a woman do if she tested positive?5
By 1999, M.K. Cho and colleagues published a study on the adoption of BRCA1/2 screening. Only 56% of physicians responding to the survey had offered the test to their patients: of those, 70% of women declined to participate citing concerns for privacy and 28% of physicians indicated that their patients had no access to genetic counselling despite the test’s requirement they do so.6
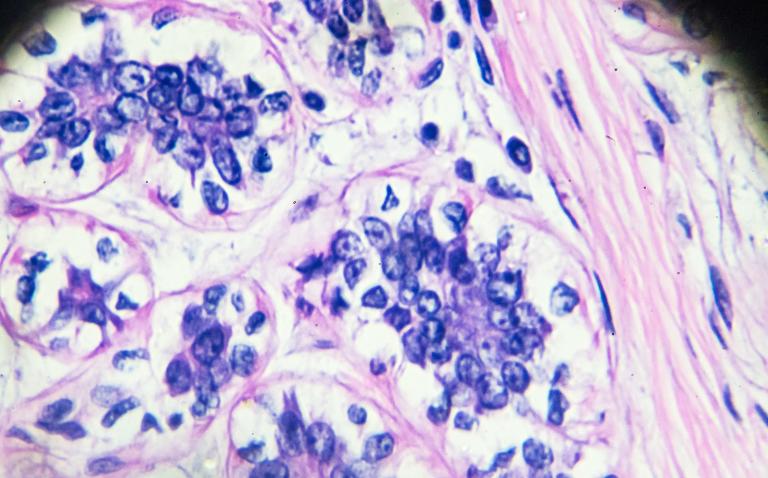
By 2009, Sir Michael Radcliffe Stratton had illustrated that cancer was the result of a series of somatic mutations,7 thus indicating that genetic screening of a single biopsy from one spot within a tumor was inadequate. His research identified the genetic heterogeneity accumulating as a result of somatic mutations. Hence the theory emerged that both germline and somatic mutation screening was required.
It took 20 years and more than 14,000 scientific papers for scientists to determine how BRCA1/2 exerted tumor suppression effects via DNA repair.8 Then David Livingston and his team showed that cells with a germline mutation in the BRCA1 gene impeded the cell’s normal function of silencing one of the two X chromosomes, hence explaining why women tended to have a higher incidence of breast cancer than men.9
BRCA testing today – the impact on treatment decisions
Germline testing is typically performed on a blood sample whereas somatic mutations are generally performed on a tissue sample (biopsy). Results of the former are combined with family history, lifestyle factors, penetrance of the mutation and other information to ascertain the risk of developing cancer. There are a number of panels now available to test for germline and somatic variations.10
In 2013, a celebrity sparked a paradigm shift in clinical decisions regarding breast cancer treatment with what is now formally known as the “Angelina Jolie Effect”. Her public op-ed announced that she underwent BRCA1/2 testing given that her mother had died of breast cancer at only 56 years old. She tested positive and elected to undergo a prophylactic mastectomy plus laparoscopic bilateral salpingo-oophorectomy. By 2016, genetic testing had spiked 285% but the number of prophylactic mastectomies remained relatively constant.11
Patients have since become aware of the benefits of BRCA testing and reconstructive post-mastectomy surgery, which has forever altered clinical decision support protocols. Patients with BRCA1/2 mutations are generally more responsive to treatment with platinum-based chemotherapy and are faring well in clinical trials with PARP (poly ADP-ribose) inhibitors. BRCA testing and treatment decisions are now inextricably linked.
Testing for BRCA1/2 mutations is a rather simple test with far-reaching consequences as women now have many options to consider from freezing their eggs, to delaying or not undergoing chemotherapy if pregnant, to life-changing surgical alterations for the patient – as well as other members of her family – all while under the increased vigilance of heightened surveillance.
BRCA testing has reached new heights. Today, clicking an ad on Facebook and $99 will trigger shipment of a cheek-swab collection tube from 23andme who obtained FDA approval for their BRCA test in early 2018. For only $299, Color Genomics will conduct a BRCA test as well as screen you for multiple other diseases. “Recreational genomics” is the newest entry into our lexicon regarding this brave new world of BRCA testing.
BRCA testing tomorrow – the future of screening
Diagnostic laboratories are now facing enormous pressure to keep up with demand, ensure the accuracy of their results and provide meaningful interpretation.12 NGS has cracked the field wide open with its high-throughput capacity to rapidly analyse large genomic regions or smaller ones for multiple samples in parallel, all without the need for detailed knowledge about the genome.13
This makes it ideally suited for familial haplotyping and hence, disease screening. NGS enabled the parallel sequencing of hundreds of breast tumors which revealed new cancer genes that were then grouped based on which pathways each mutation deregulated. The technique was then applied to further Sir Stratton’s research via the identification of mutations within a single tumor.
In essence, enabling disease monitoring at a personalised, precision medicine level. This is particularly important as variants of unknown significance (abnormalities with unknown significance to the patient’s risk for cancer) are routinely found which compromise the accuracy of the BRCA tests.
Efforts are now being made to apply and/or modify existing BRCA tests as companion diagnostics. In this way, clinicians will be able to better determine if their patients are suitable candidates for platinum, PARP or future treatment options. Longitudinal studies are now being combined with BRCA testing by Julie Palmer, a Susan G. Komen fellow at Boston University, to assess the effects on women of color, who have higher rates of breast cancer and mortality than their Caucasian counterparts. In parallel, next generation bioinformatics tools, with an emphasis on combinatorial analytics to detect multi-gene and multi-variant interactions, are under development to provide additional context and increased risk assessment accuracy of BRCA tests.
Finally, public genetic counseling centers have begun popping up (for example, the new center launched at UCSF in Feb 2018, see LINK) and will likely continue to multiply as part of the future wave of BRCA testing in order to meet the growing demands of “recreational genomics” and to relieve some of the clinical burden on physicians who still lack the required resources to manage genetic testing as part of their treatment.
With BRCA testing now a ubiquitous part of pop culture and advertising in social media, the only thing that is certain about its future is that its impact will continue to be grand. In summary, BRCA testing enables the art of the possible. Precision medicine, prevention and potentially even a cure.
References
- J.M. Hall et al.. “Linkage of early-onset familial breast cancer to chromosome 17q21”. Science Dec (1990) 250, 4988: 1684-1689.
- L.S. Friedman et al.. “Confirmation of BRCA1 by analysis of germline mutations linked to breast and ovarian cancer in ten families”. Nature Genet (1994) 8:399-404.
- Y. Miki et al.. “A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1”. Science (1994) 266 (5182): 66–71.
- M.R. Stratton & R. Wooster. “Hereditary predisposition to breast cancer”. Curr Opin Genet Dev (1996) Feb;6(1):93-7.
- R. Hubbard & R. Lewontin. “Pitfalls of genetic testing”. N Engl J Med(1996) 334:1192–3.
- M.K. Cho et al.. “Commercialization of BRCA1/2 Testing: Practitioner Awareness and Use of a New Genetic Test”. Am J Med Genet (1999) Mar 19; 83(3): 157–163.
- M.R. Stratton et al.. “The cancer genome”. Nature (2009) Apr 9; 458(7239): 719-24.
- W. Zhao et al.. “BRCA1–BARD1 promotes RAD51-mediated homologous DNA pairing”. Nature (2017) Oct 19; 550: 360-65.
- S. Ganesan et al.. “Association of BRCA1 with the inactive X chromosome and XIST RNA”. Philos Trans R Soc Lond B Biol Sci (2004) Jan 29: 359(1441): 123-8.
- G. Ellison et al.. “A reliable method for the detection of BRCA1 and BRCA2 mutations in fixed tumour tissue utilising multiplex PCR-based targeted next generation sequencing”. BMC Clin Pathol (2015) 15: 5-9.
- G. Troiano et al.. “The Angelina Jolie effect – Impact on breast and ovarian cancer prevention A systematic review of effects after the public announcement in May 2013”. Health Edu J (2017) 76; 6: 635-47.
- A. Wallace. “New challenges for BRCA testing: a view from the diagnostic laboratory”. Euro J Hum Gen (2016) 24: S10-S18.
- R. Kamps et al.. “Next-Generation Sequencing in Oncology: Genetic Diagnosis, Risk Prediction and Cancer Classification”. Int J Mol Sci (2017) 18(2): 308-12.