HOPE representatives provide information on the strategy adopted on quality and patient safety and on expectations on improving healthcare quality using patients’ experiences and competencies
Austria

Mr Nikolaus Koller HOPE Governor

Mrs Ulrike Schermann-Richter HOPE Liaison Officer, Federal Ministry of Labour, Social Affairs, Health and Consumer Protection
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
The Federal Health Commission1 adopted the Austrian Quality Strategy in 2010, which was integrated by operational objectives in 2011 to be effectively implemented. In 2012, the Patient Safety Strategy became one of the most important issues of the Quality Strategy.
It aims at the continuous further development, improvement, and nationwide assurance of quality in the healthcare sector. It supports appropriate and, most notably, reliable healthcare services provision to the population. Quality shall become the guiding and controlling criterion for the Austrian healthcare system.
The strategic objectives are:
- Continuous improvement of the process and quality results;
- Quality assurance and quality management;
- Transparency of the healthcare system;
- Risk and safety culture;
- Incentives for continuous quality improvement;
- Quality oriented training at all levels;
- Mutual support, increased cooperation and coordination of the implementation of the quality objectives at the level of the Federal State, the Länder and the social insurance.
The strategic and operational objectives as well as the actions/measures based on them are checked regularly and if needed adjusted accordingly.
Additionally, the National Framework for Healthcare Planning (ÖSG-Österreichischer Strukturplan Gesundheit) was completely revised, extended, and then republished in Summer 2017. Constituent parts of the planning guidelines are standards on infrastructural quality of healthcare settings and establishments, such as the composition, qualification and attendance of treatment teams, (minimum) equipment standards, and the particular (minimum) range of services to be provided. These standards apply to selected therapeutic areas of in-patient and out-patient care. The applicable existing legal regulations were not far-reaching and detailed enough to ensure comprehensive infrastructural quality and allow regular control and comparability.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
Patient orientation – in that patients shall be in the focus of the decisions and actions and are enabled to take an active part – is essential in making efforts to improve quality of care.
Active participation, however, requires a certain degree of personal competence and responsibility. Thus, in order to empower people to be actively involved, strengthening the health literacy of the population and vulnerable groups by appropriate measures is a declared common goal of the health reform partners over the next four years. The measures envisaged include the enhancement of independent information in the internet health portal (www.gesundheit.gv.at) on health and diseases as well as on possibilities of healthcare provision, available evidence of treatment options, and on the functioning of the healthcare system. Additionally, there will be standards developed on how written information on health issues can become most clearly understandable. In order to improve the oral communication between patients and healthcare providers and support both in being ‘partners’, healthcare providers will be trained to improve their communication skills.
It was also agreed to continue the regular cross-sector surveys on patient satisfaction with the service provision in the healthcare system.
The survey captures the patients’ experiences on care processes, in particular the communication and care processes at the interfaces. Data suggests that patients’ involvement in care processes may bring about an optimisation in the healthcare service provision. Surveys repeated on a regular basis allow for the monitoring of services and evaluation of improvement measures set. Patient experiences and opinions thus become the starting point for quality improvements and for the optimisation of patient pathways in the healthcare system.
Denmark

Mrs Eva M. Weinreich-Jensen HOPE President, Danish Regions
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
Quality and patient safety are very important in the Danish Quality approach. Denmark established the National Quality Programme in 2016. It aims explicitly at building a nationwide improvement culture through eight national targets and a number of indicators, interdisciplinary collaborations and a national leadership programme. The approach is based on a close cooperation among the State, the regions and the municipalities. The goal is putting patients first and improving the results for them.
The programme replaced the accreditation in hospital and pre-hospital settings. Each hospital and region set their own goals in relation to the overall national targets based on the challenges they face. National learning initiatives and collaborations are established, with the aim of improving the clinical quality result in specific areas, and the experience for the patients and their relatives. In many ways, though, the work on quality was handed back to clinicians. This shall be interpreted as an act of confidence towards the health professionals and their inherent ambitions to improve clinical quality.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
Improving the quality of healthcare using the experiences and competencies of patients is a central feature of the Danish approach. Patient safety is one of the eight national targets. Some examples of initiatives implemented in this regard are the use of patient-reported outcome measures (PROMs) and of surveys on patient satisfaction covering many areas of the healthcare sector such as emergency care, psychiatry and maternity wards. Better continuity of care and improved patient involvement are two further national targets. “It is common understanding that the improvement of results for patients is the core of our daily activity. It is not as simple to accomplish it as it sounds, but the dedication is there. By keeping a close eye on the development within the targets we believe, we will come far along this new path”.
Estonia

Mr Urmas Sule HOPE Vice-President, Estonian Hospitals Association
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
Estonia held its first term as the presidency of the Council of the EU from July to December 2017 during which the priority was to enhance cooperation on eHealth among member states and to reduce alcohol-related harm. The overall aim was to come to an agreement to reach Council conclusions to tackle these subjects.
Digital solutions provide people with better opportunities to take care of their health and help health professionals to improve the quality of treatment. Digital solutions allow patients to be more involved in decision making about their health and to make treatment more accurate and better tailored to individual needs. Citizens must have the right and opportunity to digitally access their health data, as well as to allow or restrain the safe sharing of health data for the use of various e-services.
“We have kept developing our eHealth systems during the last decade and we believe this has a huge impact on healthcare, including patient safety”.
The largest eHealth project is the introduction of the electronic health records system. This project aims to develop a basic infrastructure for the integration of healthcare providers’ data. The digital images, digital registration, and digital prescription projects use the same message administration, authorisation, central data storage, and other services created in the framework of the electronic health records project.
For a long time, Estonia has been tackling problems caused by alcohol consumption. The Estonian government has approved stricter alcohol policy and new laws to protect the country and, most importantly, the health of the youth by implementing restrictions on alcohol availability and its sale and advertisement. It has already changed people’s attitudes towards the display and availability of alcohol and made people seriously consider reducing their alcohol consumption.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
Patient-centred care has been discussed and developed in different medical areas in Estonia for many years. Involving patients in their personal health development is a more successful way to achieve results than simply letting the doctor treat their disease. Patient centred healthcare improves the quality of treatment, has a positive effect on patient health and increases his/her satisfaction with treatment.
Patient-centred healthcare is the way to a fair and cost-effective healthcare system. Globally, health systems are under pressure and cannot be sustainable if they continue to focus on diseases rather than patients. They require the involvement of individual patients who adhere to their treatments, make behavioural changes and self-management. Patient-centred healthcare may be the most cost-effective way to improve health outcomes for patients.
To make this happen, all stakeholders in the healthcare field, including the patient, must change their attitudes and behavioural patterns. The patient takes responsibility for self-educating about different treatment options, participates in choices and follows the agreed treatment, changing the attitudes and behaviour accordingly.
The Estonian Ministry of Social Affairs started a Patient Safety Development Initiative, dealing with the main issues related to patient safety, the green paper on quality and the Patient Insurance Act. Currently this act is in the development phase. The aim is to reduce the risk of doctors’ fear of potential legal liability to a minimum, which would enable them to focus more on patients’ effective medical treatment.
Finland
Mrs Hannele Häkkinen HOPE Governor, The Association of Finnish Local and Regional Authorities
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past 10 years?
According to the Healthcare Act (No. 1326/2010), Section 8 on quality and patient safety, the provision of healthcare services shall be evidence-based. The healthcare services provided shall comply with the highest quality standards and be properly organised. Each healthcare unit shall produce a plan for quality management and for ensuring patient safety. The plan shall include arrangements for improving patient safety in cooperation with social services. The issues to be covered in the plan are laid down by decree of the Ministry of Social Affairs and Health.
The Patient Safety Strategy has been released for the years 2017–2021. It will help to develop a cohesive safety culture.
Disease-specific quality registers are patients’ groups or disease-specific care monitoring systems that support the daily care of patients. They gather structured clinical data that can be used for monitoring the effectiveness and quality of treatments. Disease-specific quality registers are being used to monitor 52 disease groups.
A register for 27 additional groups of diseases is under development.
HaiPro is a web-based tool for reporting patient safety incidents. It is used by over 200 social service and healthcare organisations of various sizes: from small healthcare centres to entire hospital districts. The HaiPro reporting system supports the development of procedures within the organisation.
The Healthcare and Social Services Act, stating the division of activities among hospitals, emergency services, first aid and emergency social services has been reformed in 2018. The objective is to guarantee equal access to services, sufficient skills and knowledge, patient safety and to decrease health expenditure.
The Health and Social Services Act reforming process is ongoing.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
In Finland, the patient orientation is highlighted in healthcare planning, implementation and evaluation. Patients have been involved as experts in government working groups. The development of healthcare and social welfare provision will be based on patients’ experiences and participation.
One of the government key projects is the establishment of a model based on expert’s experience and patient involvement. In Central Finland Healthcare District, forms of co-design have been developed in specialised medical care, primary healthcare, social welfare and municipal welfare work. The aim is to increase patient and citizen participation in planning, preparation and evaluation of healthcare services by collecting feedback on their experience. A model of co-design for patient-driven self-management of non-communicable diseases was developed. Observations based on expert experience in psychiatric departments were provided in 2017.
In Satakunta Hospital District, a patient panel participated in the planning and construction of a new hospital. The panel gathers patients’ feedbacks to develop services and products and to create or test new ideas.
One of the government key projects is the development of virtual hospital services. Finnish university hospitals are building a joint national virtual hospital, which, in practical terms, means a digital service hub for specialist healthcare. It aims to develop patient-oriented digital healthcare services for citizens, patients and professionals.
The project, which runs from 2016 to 2018, is a joint initiative coordinated by the Helsinki and Uusimaa Hospital District HUS. In developing digital healthcare services, the patients and their needs define the core of the service and the value chain that is built around it. In the Virtual Hospital 2.0 project, the patient’s voice has been affirmed in such a way that the current e-service development model brings patients, their close friends and patients’ organisations into service planning and design.
Inclusion methods are based on patients’ interviews, service design workshops, participation at working groups, and patient relationship management. The service design also includes experienced experts, peer educators, and specialist patients’ organisations.
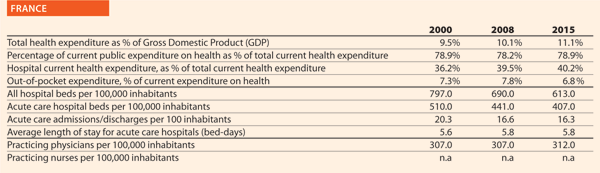
France

Mrs Zaynab Riet HOPE Governor, French Hospital Federation (FHF)

Mr Antoine Perrin Chief Executive, French Federation of Non-Profit Hospitals (FEHAP)

Mrs Pascale Flamant Chief Executive, French Federation of Comprehensive Cancer Centres (UNICANCER)
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
For the last ten years, the High Health Authority (Haute Autorité de Santé – HAS), has been producing guidelines on a number of topics, in collaboration with learned societies. Furthermore, every hospital has to be evaluated and certified by HAS regarding safety and quality. Efforts have been made to introduce patient centric procedures, that led in turn to a decrease of severe adverse events. Patient satisfaction is measured by the hospital
and contributes to a better fit between patient expectations and medical procedures.
Simultaneously, the Health Ministry and the French National Sickness Fund put in place policies and programmes aimed at reducing the number of unnecessary medical procedures, most notably through monetary penalties. An atlas on variation of medical practices has been produced, focusing on nine procedures. It shows huge geographical variations, pushing hospitals and providers to search for explanations of these variations.
Enhanced recovery programmes are identified as a major axis of development of oncology in France. Therefore, many French comprehensive cancer centres have now implemented, or are about to implement, those programmes to meet cancer patients’ wishes to safely go home shortly after surgery. The programmes, coordinated by a healthcare professional, cover the patient pathway and provide different measures, such as:
- Preparing the patient for surgery (management of anaemia, physiotherapy, etc)
- Managing the patient’s pain during surgery (including epidural analgesia)
- Activities from the first postoperative day (early ambulation, physical activity with pedal exercisers, etc).
Eight French comprehensive cancer centres have been labelled as reference centres by the Francophone Group of Improved Rehabilitation After Surgery (Groupe francophone de Réhabilitation Améliorée Après Chirurgie – GRACE).
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients
Despite the efforts of the Health Ministry, Sickness Fund and HAS, in the implementation of programmes relying on penalties, success remains somewhat limited, in large part because of a lack of appropriation by front-line clinicians. The approach adopted is ‘top-down’.
Since 2015, the French Hospitals’ Federation (FHF) is part of ‘Choosing Wisely’, an international campaign launched in the US and Canada, which aims to improve the dialogue between patients and clinicians on the topic of relevance. Since 2017, the FHF is the national leader for this campaign. Learned societies as well as patient associations have since then started working on ‘Top 5’ lists.
A national logo has been created, and the construction of a website is under way. The lists will be displayed on the website and will be accessible by providers and patients alike.
One of the first of these lists, concerning geriatrics, has been tested in all of the hospitals of the Region of Brittany, and three of the five items have shown their relevance and robustness. Work has been undertaken to improve the quality of recommendations and their understanding by patients. The FHF provides technical support in the process and helps to create consensus regarding the items that will constitute the Top 5 lists.
A national advertising campaign will be launched in hospitals as well as in non-hospital settings in GP’s offices. Around 20 learned societies are already part of the campaign.
The FHF is also working with the Deans of Medical schools to introduce ‘Choosing Wisely’ in the medicine curriculum, as well as to organise activities around this theme involving French and foreign students.
In 2017, UNICANCER launched a project that aims to facilitate the communication between cancer patients and their healthcare professionals. The idea of the initiative is to set up a digital tool, collecting data on the patient experience on consultations during their treatment for cancer. The survey has met with good success, from the perspective of both patients and doctors, allowing the patient experience to be brought to light to help medical decisions. The project will be extended to further comprehensive cancer centres that volunteer to participate.
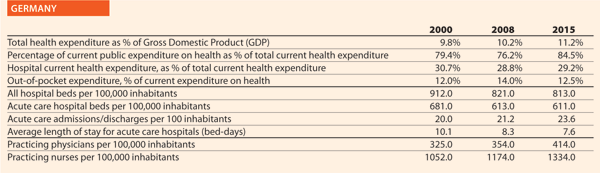
Germany

Mr George Baum HOPE Governor, German Hospital Federation
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
German hospitals are continuously working on improving quality of care and patient safety. They actively apply CIRS – Critical Incident Reporting System (sharing evaluated experiences with colleagues and other hospitals) at hospital wards, at local, regional and national level and support the National Action Alliance on Patient Safety (campaigning for safety issues, for example, hand hygiene).
Additionally, several legal initiatives have been implemented. Hospitals are assessed annually on approximately 400 quality indicators by an external institute and receive a report that has to be published. The data of this so-called ‘system of external quality assurance’ serve as a basis for the official hospital directory and search engine for patients, and encourages doctors to provide a very high level of transparency and quality. The IQTIG (Institute on Quality and Transparency in Healthcare) will soon provide an objective quality criterion for ‘pay for performance’ and for hospital planning. Minimum volumes for provision of healthcare services are defined and minimum numbers of staff for intensive care services are defined. Finally, hospitals provide comprehensive discharge management services to their patients.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
Hospitals are conducting voluntary patient surveys aimed at collecting feedback on their experience concerning all aspects of their stay (for example, personal satisfaction with admission procedures, information and communication by the hospital, accommodation, quality of the staff or of the catering, waiting times and hygiene).
In certain circumstances, these interviews are also addressed to the relatives and partners of patients. Some of these surveys are also used for benchmarking. In addition to this voluntary assessment of patient satisfaction, hospitals are asked to question patients on different services by the Federal Joint Committee as part of the mandatory quality assurance system on the basis of an interview form developed by the IQTIG.
German hospitals also have patient advocates who assist patients in representing their interests. Acting independently in the hospital they moderate between healthcare providers and patients. As this option was given by law, some Federal States have already developed recommendations for them, providing both framework and contents for their duties and rights. Additionally, hospitals have for some time also applied complaint management systems. They provide options for patients to complain anonymously about all aspects of their treatment. This feedback delivers valuable information for hospitals on how to improve services.
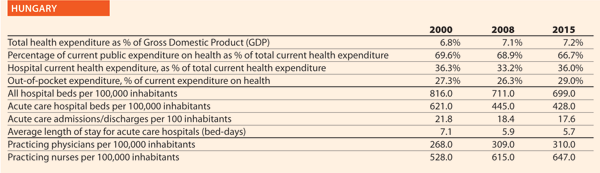
Hungary

Mr György Velkey HOPE Governor, Hungarian Hospital Association
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
The aim of old quality assurance systems was to regulate the healthcare processes, which would have led, in turn, to better results in the future. The new approach shifted the focus to the final result instead: patient safety. This means that all healthcare processes have to be planned and structured in the light of all potential risks that can pose a threat to the patients, starting from the purchase of healthcare materials. This challenge is addressed by the new ISO 9001:2015 standard.
The majority of Hungarian hospitals operate by ISO-certified quality assurance systems. However, with the use of EU resources, the Hungarian Government managed to set up a customised standard framework (called BELLA) in 2014, which is in line with the international quality requirements (ISQua) and focuses on patient safety.
The Hungarian Hospital Association supports the new quality assurance methods. Hospitals are applying indicators which are suitable for monitoring patient safety and its shortcomings, partly following-up on own data and comparative analysis based on information gained from other similar institutions. The main points of the new system are continuous learning and self-assessment which is, of course, challenged by an external review once a year. The process of accreditation is being elaborated at the time of writing (January 2018) and will be ratified. An online tool (NEVES) is maintained for reporting all unexpected (adverse) events.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
In-patients participate in a pre-organised and personalised counselling session before they leave the hospital. The person who is responsible for this tailored service has to be sure that the patient has understood all the advices regarding healthy living, physical exercise, physiotherapy, diet, and use of medical devices. Patients are free to ask questions. Healthcare providers have to certify all these aspects in the final report. Hospitals operate a well organised system for the management of patients’ complaints and comments.
Several staff members are involved in the investigation of complaints. However, it is the managing director who makes the decision. There are independent patients’ rights commissioners in each hospital, representing patients’ interests in problematic cases and supervising the fairness of the investigations. The leadership looks into all the complaints annually and suggests development measures when needed. Hospitals run their own web pages, which aim to provide information but also work to receive information and feedback from the patients.
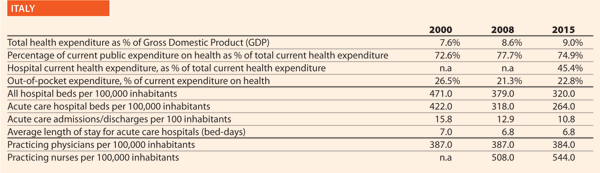
Italy
Mr Domenico Mantoan HOPE Governor, Veneto Region
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
Quality and patient safety are prominent issues of the Italian health policy. National legislation states that patient safety is in itself a part of the right to health. Promoting quality means to promote a multi-sectoral strategy, involving staff, patients, strengthening a safety-culture which would be incorporated in each health organisation. Many actions addressing towards this direction, are stated by Italian National Law for monitoring sentinel and adverse events, supporting risk management, promoting training and education for staff and education for patients.
With regards to monitoring, since 2009, National law states that hospitals and healthcare trusts have to monitor sentinel events, transmitting specific reports to the National Health Ministry.
Another important initiative, the National Outcome Evaluation Programme, started in 2011, has been promoted by Agenas (National Agency for Regional Health Services). Agenas collects records from hospital trusts and health local trusts and calculates specific indicators of quality, such as the percentage of femur neck fractures being treated by surgery within two days, and the percentage of AMI being treated by PTCA within two days.
The aim is monitoring quality of care by means of indicators coming from a routine database so that this monitoring has to be incorporated in the control system of each health organisation, on a regular basis.
Regarding a multi-sectoral approach, the most advanced experience is the Pilot Project CARMINA, started in 2010 and supported by the National Health Ministry. It is based on a self-assessment questionnaire aimed at evaluating the level of patient safety of an organisation. Each health organisation is tested through 52 items covering the following main areas: safety culture, communication, human resources, safe environment and safe contests, care processes, management of adverse events, and management of health records.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
Using patients’ experiences and competencies along with other components such as effectiveness and safety of care are essential for providing a complete picture of healthcare quality. This is helpful to get a better patient compliance in the treatment: listening to patient experience is important for providing an effective and anticipatory guidance to establish a health maintenance and management plan to promote health and to prevent potential problems.
This means, also, that the patients (or designee) are recognised as a source of control and a full partner for providing compassionate and coordinated care based on patient values, needs and preferences. Moreover, it is important considering several aspects of healthcare service provision that patients value highly such as: getting timely appointments; providing easy access to information; providing good communication between staff, patients and care-givers.
In Italy, patients’ representatives are involved in many working groups and/or projects such as pain free projects, specific disease projects (for example, diabetes treatment), health promotion projects and waiting list working groups. The aim is to create an appropriate health culture, which is very important considering the potential overexposure of patients to health information that is often fake news.
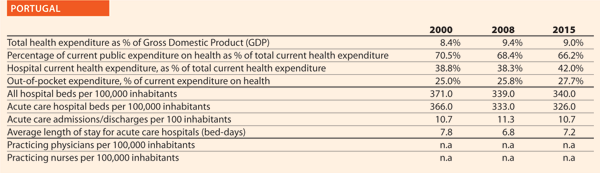
Portugal

Mr Carlos Pereira Alves HOPE Governor, Portuguese Association for Hospital Development
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
Over the last ten years, the strategy adopted by the Ministry of Health in Portugal included several structural initiatives:
- The creation of the Department of Quality in Health in the General Directorate of Health, in 2009;
- The adoption of the 2009–2014 and the 2015–2020 National Strategy for Quality in Health that includes the 2015–2020 National Plan for Patient’s Safety;
- Adoption of the ACSA certification model for the institutions of the National Health Service;
- Creation of Safety and Quality Committees in all hospitals and primary healthcare units functioning as a network with the Department of Quality in Health;
- Articulation between the Ministry of Health and the medical association to develop clinical guidelines and perform audits to clinical standards;
- The creation of the National Incident Reporting System available to citizen and healthcare workers, in 2011;
- The development of the pilot-project “Patient Literacy for Healthcare Safety”.
The Ministry of Health, through the annual reports of the Safety and Quality Committees, monitors the development of quality and patient safety activities in the national healthcare institutions. These are: national guidelines adopted and audits performed in the institution; certification of healthcare units and institutions; safety culture assessment; communication safety; surgical safety; safe use of medicines; identification of patients; notification and risk management; prevention and control of infections and antimicrobial resistance.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
The main expectations on improving the quality of healthcare using the experiences and competencies of patients are:
- To improve patient’s literacy on safe delivery of care;
- To increase the participation of patients in the healthcare service provision, as an active team member;
- To improve safety culture in the healthcare institutions.
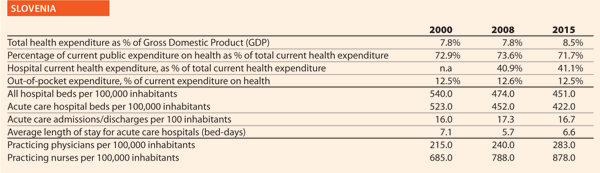
Slovenia

Mr Simon Vrhunec HOPE Governor, Association of Health Institutions of Slovenia
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
Approximately 15 years ago, the Ministry of Health introduced the programme of quality improvement in the health sector. For that purpose, the Department for Quality was established. First, a set of quality indicators was developed with the cooperation of the Institute for Public Health of the Republic of Slovenia and the hospitals themselves. Hospitals were obliged to collect data and to report indicators to the Ministry of Health. In this period, the ‘non-blame culture’ was developed in hospitals. Moreover, the quality indicators were published and made available on hospitals yearly reports. Finally, the Ministry published each year a brochure with indicators for all hospitals.
In 2012, the Ministry of Health and the Health Insurance Institute of Slovenia agreed that hospitals should have been accredited by an international accreditation model by the end of 2014. For hospitals not accredited by that date, it was decided that the price for services would have been decreased for 0.3%. Hospitals were allowed to choose the accreditation model by themselves. Most of them decided for DNV-GL accreditation, the other decided for JCI. Since 2016, this obligation does not now exist. Some hospitals still have their accreditation model established and others have decided to use ISO 9001 and ISO EN 15224. Health institutions are still facing some blame from media and the general public for the adverse events reported.
In 2017 Ministry of Health initiated the so-called Šilih project. The main purposes are to identify and validate measures to reduce and prevent warnings and adverse events during medical treatments; to exercise the right to adequate, high-quality, and an effective judicial procedure when mistakes occur.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
In Slovenia there is a big gap between expectations of the population regarding healthcare services and the possibility of public financing to assure those services. The results of this gap are very long waiting lists and waiting times for specific services. Emergency care is provided immediately. For all elective services, regardless if they are needed with urgency, the providers (hospitals) cannot assure them in reasonable time. Spine surgery represents one of this cases. Waiting time for service differs among hospitals and varies from six months to more than two years. It is a reasonable expectation of patients and healthcare providers that government should address its resources (financial and human) to decrease waiting times. Since public opinion is that providers are responsible for waiting times regardless of the fact that these are actually caused by a lack of resources, hospitals also expect that Government would accept the responsibility. The other expectation of the providers is to start to rebuild a ‘non-blame culture’ because the trust between patients and providers is at its lowest-ever level and consequently it is very hard for healthcare professionals to work in such circumstances.
In the past in the University Medical Centre of Ljubljana, there was a board of patients nominated to improve the management of processes, taking into consideration their experiences. This is a good example of patient empowerment.
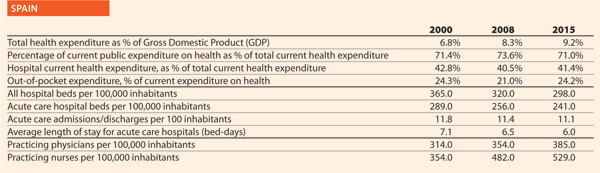
Spain

Mrs Sara Pupato Ferrari HOPE Governor, Ministry of Health, Social Services and Equality
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
The Ministry of Health, Social Services and Equality (MSSSI) fosters and promotes the Patient Safety Strategy for the National Health System, which has been carried out since 2005 in collaboration with the Health Regions and the National Institute of Health Management (Instituto Nacional de Gestión Sanitaria – INGESA), integrating the contributions of the healthcare professionals and of the patients through organisations representing them.
The objectives of this strategy aimed initially at: promoting and enhancing patient safety culture in the healthcare organisations; incorporating risk management practices; training the professionals and patients on basic aspects of patient safety; implementing safe practices and getting patients and citizens actively involved.
The Patient Safety Strategy has been extended for further five years (2015–2020) to provide an overview of what has previously been done and to facilitate decision making based on consensus. Furthermore, the strategy has been evaluated positively showing that the established collaboration with the Health Regions has worked efficiently. The contributions of the professionals and their organisations turned out to be crucial and the scientific societies have played a key role. Finally, the patients and their representatives contributed to patient empowerment.
The update presented herein incorporates the strategic actions set out, including the international recommendations and the achievements and objectives defined on the base of available evidence. The team that contributed to shape the strategy is composed of scientific and technical coordinators and the institutional technical committee of the Health Regions.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
Spanish Network of Health Schools for Citizens
This network provides patients, family members and care-givers with a source of information and training services, giving them access to the best scientific evidence available. It is based on the contributions of various schools and projects within the National Health Service (Escuela Andaluza de Pacientes, Escuela Cántabra de Salud, Escuela Gallega de Salud para Ciudadanos, Programa Paciente Expert Catalunya, Programa Paziente Bizia Osakidetza) along with the Citizen Training Network of the National Health System, the Ministry and the Foundation of Health and Ageing of Autonomous University of Barcelona (Fundacio Salui i Envelliment – Universidad Autónoma de Barcelona – UAB). It also receives contributions from patient and professional associations.
Patient as auditor
The European Council and the WHO World Alliance for Patient Safety stress the importance of the engagement of patients and their relatives in the improvement of healthcare safety. Many initiatives have been studied to support patient engagement and to face this challenge. Nevertheless, the role of patient as auditor of safety practices remains almost unexplored. It consists of voluntarily and anonymously tracking clinical practices.
Some of the suitable practices in which to engage the patient as auditor are those that require an external observer (hand hygiene, patient identification, transfusion, chemotherapy administration, etc.). The adherence to those safety practices cannot be measured by analysing data gathered through the information system. For example, it is possible to detect a wound infection but not if the healthcare professional washed his/her hands before or after the contact with the patient.
The role of patient as auditor does not imply that he/she has to take an active role reminding the healthcare professional to follow a safety practice (for example, the patient reminding the nurse or doctor to wash their hands if they did not).
It requires the patient to assess if the professional follows the procedures in normal conditions.
To explore the feasibility and validity of patient participation as partner in the audit of safe practices, the Navarra Complex Hospital (Complejo Hospitalario de Navarra) is performing an innovative project composed of several stages. They are developing some learning materials while evaluating the feasibility and validity of the patient as auditor. Furthermore, they are exploring the experiences and perceptions of patients, professionals and managers about the role of patients as safe practices auditors.
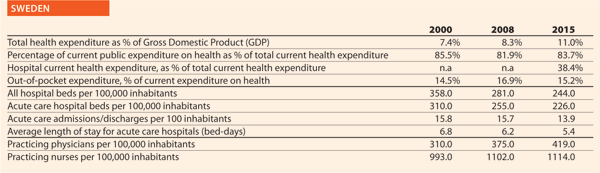
Sweden

Mr Erik Svanfeldt HOPE Governor, Swedish Association of Local Authorities and Regions (SALAR)
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
One important initiative on quality in the healthcare sector was the annual open regional comparisons of healthcare quality and efficiency, that the Swedish National Board of Health and Welfare and SALAR started to publish annually in 2006. SALAR now provides such statistics online at vardenisiffror.se.
The purpose was to make the publicly financed healthcare system more transparent, promote healthcare management and control, and to contribute to improved data quality and simplified data access. The comparisons are based on several different indicators reflecting various dimensions of quality and efficiency such as medical outcomes, availability, patient experience and costs. Different sources are used, like the national healthcare quality registries and population/patient surveys.
Comparisons have changed the perspectives, by giving attention to differences in medical results and outcomes, and revealing regional differences concerning quality of care. Now the debate is not just on compliance to budget, but also to a larger extent on quality issues.
Patient safety has been on the Swedish policy makers’ agenda for several years. From the early 2000s, SALAR put in place a number of actions that were further accelerated by a four-year agreement signed in 2011 between SALAR and the Swedish Government. This national initiative highlighted healthcare-associated infections, fall injuries, pressure ulcers, malnutrition, medication errors, and antimicrobial resistance. In 2010, a new Patient Safety Act was also introduced, promoting among other things proactive work, risk reduction and patient involvement.
Great progress has been made over the past years. A robust infrastructure for patient safety efforts has been implemented, the use of antibiotics has been reduced and the number of severe adverse events has decreased. But to further improve patient safety, SALAR, together with counties, councils/regions and municipalities, developed a National Framework for Patient Safety in 2015 to foster strategic working.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
SALAR strongly believes in the involvement of patients and their relatives as active partners in the planning, implementation, development and follow-up of healthcare operations. Today, better educated patients want to be involved – and should also be encouraged to get involved – both in their own care process and in the operations in general.
Patients and relatives have lots of experiences and competencies that the health systems should take advantage of and use in the designing of health services. By using patients’ knowledge, views and experiences at both individual and aggregated level, the healthcare services can be improved.
In Sweden, this is done through national patient surveys, patient involvement in decision making and regional patient advisory committees.
“We believe in a relationship between healthcare professionals and patients that encourages feedback and patient responsibility for health prevention, medical treatment, diagnostics, monitoring, and self-reporting of health data. We can see a lot of benefits having more motivated and engaged patients with increased understanding, and by that being able to have a more open dialogue with the healthcare professionals. We also expect patient participation to contribute to better patient safety and improved healthcare quality. Making the patient an integral member of the team, contributes to new progresses in the fight against adverse events. All national quality registries have PROMs, and all registries also have patient representatives in the steering committee”.
One way to encourage patient participation is to develop and invest in new digital solutions. New digital tools can give people more influence, and also greater opportunities to take responsibility for their own healthcare. SALAR is involved in the management and development of the Swedish nationwide web portal 1177.se, which purpose is, among other things, to improve access to correct scientific health-related information and increase health literacy, but also to facilitate patients’ access to their own electronic medical records.
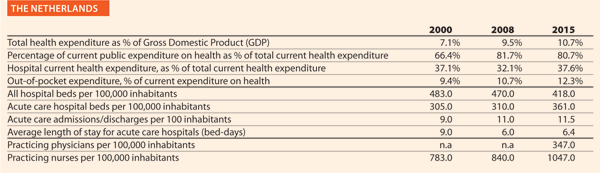
The Netherlands

Mr Sander Gerritsen HOPE Governor, Dutch Hospital Association
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
To embed patient safety in healthcare practices, all Dutch hospitals have an accredited or certified Safety Management System (VMS in Dutch). Through this system, hospitals continuously identify risks, implement improvement, establish, evaluate and modify policy. The programme (2008–2012) has led to a large reduction of avoidable damages and mortalities. From 2012, parts of the programme continued as the Safety Agenda, focusing on three pillars: medication safety; the safe application of medical technology; and infection prevention/antibiotics.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
Patient involvement is not an end in itself. It is a promising way of increasing patient safety by making use of knowledge and experience of patients. After all, patients view situations from a different point of view and they are the only ones who complete the entire care process.
“This approach is an essential addition to your own perspective. We believe the patient should be actively and systematically involved when drafting, executing and evaluating patient safety policy. Patient involvement is one of the basic demands in the Safety Management System”.
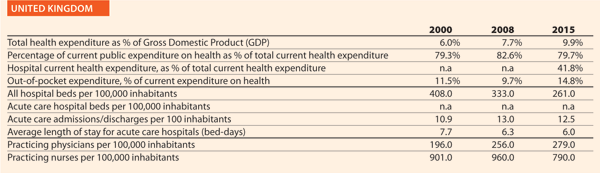
United Kingdom

Mr Niall Dickson HOPE Governor, NHS Confederation
Could you outline the strategy/approach adopted in your country on quality and patient safety or the two/three initiatives in the hospital and healthcare sector in the past ten years?
The Care Quality Commission (CQC), a quality regulator established as part of wide-ranging reforms to the NHS in 2012, has had major impact on the approach of the NHS to quality and patient safety. The CQC developed a new inspection regime for hospitals and other trusts in the NHS, providing ratings under five different domains, one of which is safety. Trusts performing poorly are placed in ‘special measures’ and offered additional support to improve care. These changes have been credited with focusing the minds of hospital boards on safety, with 16 of 31 Trusts placed in special measures having moved out of this programme after improving the quality of care.
Another pivotal influence on patient safety has been the final report of the Mid-Staffordshire NHS Foundation Trust Public Inquiry. Published in 2013 in the wake of a serious patient safety scandal, this report has shaped much of the direction of patient safety initiatives in recent years. Its wide ranging recommendations focused particularly on the importance of openness, transparency and candour throughout the health service. This led to a number of legislative changes and an increase in nursing staff numbers in the acute sector.
In 2012 the UK was first the country in the world to introduce medical revalidation – whereby every practising physician is subject to an annual check on his/her performance. This applies to all doctors whether they work in the public or private sectors. Every five years each doctor has to be signed off by a Responsible Officer (a senior doctor) who has statutory authority to recommend (or not) to the regulator (the General Medical Council) whether the doctor should retain his or her licence. The programme has stimulated a major reform of clinical governance arrangements in the UK healthcare systems.
In addition, the government is currently considering a new bill on Health Service Safety Investigations. This Bill would establish an independent investigations body to respond to healthcare errors, finding answers and helping to embed new practices. The ‘no blame’ approach will aim to mirror the practices of the Air Accident Investigations Bureau, allowing individuals to share information freely without fear of disclosure in order that investigations can find answers quickly and accurately.
Could you present us the two/three expectations that your organisation/country have today on improving the quality of healthcare using the experiences and competencies of patients?
Patient involvement and experience are built into the NHS national contract and so must be included in hospital’s quality plans at a local level. They are also built into the competency frameworks of local commissioners (CCGs).
In addition, the quality regulator, the CQC, recruits members of the public to act as “experts by experience” as part of their inspection regime. These individuals may use health services themselves, for example those in the early stages of dementia, or with a learning disability, sensory impairment or mental health condition. They may also be carers for people who use health services. Children and young people who use services and those who have recently used maternity services are also encouraged to get involved. Experts by experience attend inspections of health and care services, talking to staff, patients and families and observing how services are delivered. Their feedback is then used to support and inform the judgements of inspectors. Patient involvement is part of the CQC framework for assessment, so these inspections will also be looking at how effective the organisations they inspect are at involving patients.
Another organisation that seeks to use the experiences of patients to improve services is HealthWatch. They act as a “consumer champion” for health and care services to help ensure that patients’ experiences are heard and used to influence those with power to implement change.
The NHS in England runs a number of surveys including the friends and family test (REF), which assesses whether patients and staff would recommend the institution to their loved ones. Independent of government but now well used within the NHS are various means of collecting contemporaneous patient feedback. The company Iwantgreatcare.com enables patients to rate their doctor and also operates in hospitals with patients able to comment on nursing and other aspects of care. There has been some resistance from the medical profession to certain aspects of this very public form of assessment, but the direction of travel is clearly towards greater transparency about the performance of both individual professionals and the institutions and systems in which they work.
Reference
- Back then, the Federal Health Commission consisted of representatives of the Federal State, the Länder, the social insurance, the cities and municipalities, the confessional hospitals, the patient advocates and the chamber of doctors.










