Bronchiolitis is a lower respiratory tract infection. It results in an episode of wheezing in children in their first year of life. It is subject to seasonal variation, peaking in winter months.1–4
Respiratory syncytial virus (RSV) is the commonest causative organism, but other respiratory viruses are attributed to the disease.1–4 After a steady increase over the past 20 years of cases requiring admission, recent data suggest a plateau.1
Guidance
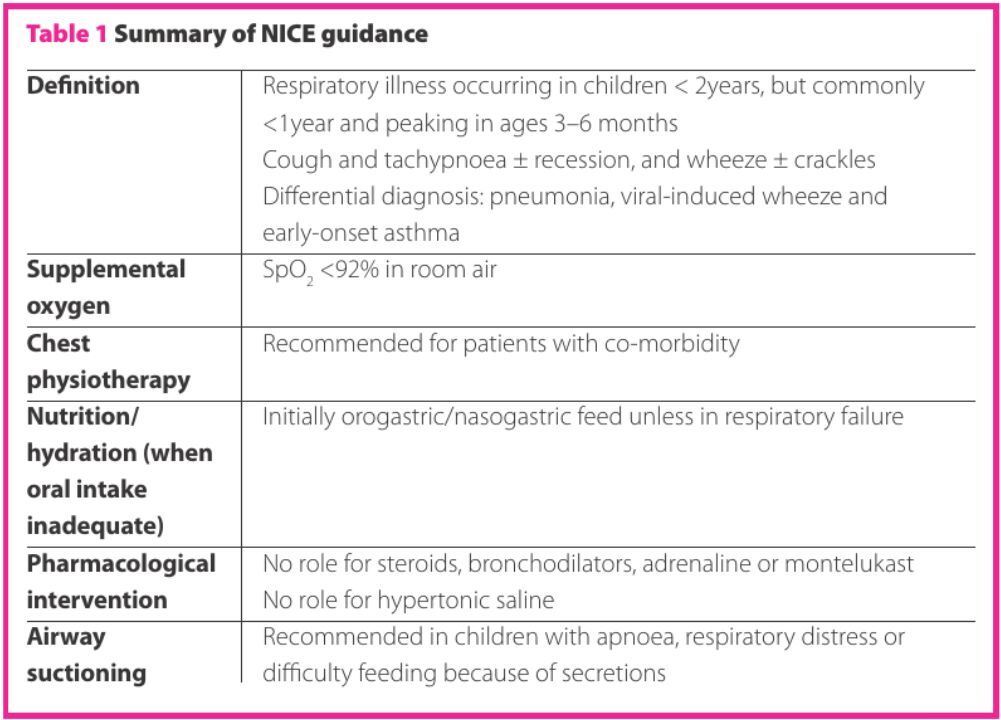
The National Institute for Health and Care Excellence (NICE) published their first guideline on bronchiolitis in 2015.1 NICE recommendations are based on systematic reviews of current evidence on best practice weighed against cost-effectiveness. The guideline was developed by the National Collaborating Centre for Women’s and Children’s Health and covers diagnoses and management of bronchiolitis. It is aimed for professionals in primary and secondary care.
Previous guidelines have been published by the Scottish Intercollegiate College Network (SIGN) in 2006, detailing diagnosis, management and prevention of bronchiolitis.2 The American Association of Pediatrics (AAP) published a similar guideline in 2014.3 The NICE guideline does not discuss strategies to limit spread of the disease or targeted palivizumab immunisation, which are discussed in the guidelines published by SIGN and the AAP.3,4
Highlights from the NICE guideline are summarised in Table 1.
Key priorities for implementation
- Identify those at risk of severe bronchiolitis
Patient groups considered to be at risk include: children with chronic lung disease; congenital lung disease; congenital heart disease; infants less than three months old; and infants born <32 weeks gestational age. Children with neuromuscular disease or immunodeficiency are at particular risk if they have bronchiolitis. Admission should be considered if they present to secondary care.1
- Signs of severe disease
Children with worsening respiratory distress, decreased fluid intake below 50–75% of normal, no wet nappy for 12 hours, apnoea, cyanosis or exhaustion should be brought for prompt clinical review.1
- Pharmacological treatment
Apart from oxygen supplementation if percutaneous oxygen saturation (SpO2) is <92% in room air, there is no evidence for pharmacological treatment such as antimicrobials, adrenaline, hypertonic saline, salbutamol, montelukast, ipratropium bromide, systemic or inhaled corticosteroids in the management of bronchiolitis.1–3
- Discharge
An infant who is clinically stable, is tolerating feeds and has had SpO2 >92% in room air for more than four hours, including during a period of sleep, should be considered for discharge. It is important to provide information on avoiding environmental smoke exposure because of its deleterious effects on a child with bronchiolitis.1
- Investigations
The diagnosis of bronchiolitis remains clinical, and hence the pertinence of recognising those in need of referral to secondary care. Percutaneous saturation measurement (SpO2) <92% is an indicator, as is apnoea, severe respiratory distress, central cyanosis, and inadequate fluid intake. Routine chest radiographs, blood or capillary gas testing and testing for viral cause should not be performed routinely.1,4
- Management
The cornerstone of bronchiolitis management remains supportive; to maintain hydration and saturation.1 There is no curative therapy.4
Supportive fluid management with orogastric (OG) or nasogastric (NG) feeds for those with inadequate fluid intake should be considered, and intravenous fluid for those who cannot tolerate OG/NG feed or who are in respiratory failure.1
NICE recommends that supplemental oxygen should be administered at SpO2 <92%. However, there is a lack of evidence as to the optimal target SpO2 for supplemental oxygen therapy for bronchiolitis. A double-blind randomised equivalence trial published in 2015 compared SpO2 90% versus SpO2 94% as thresholds for supplementary oxygen. The study concluded that a target SpO2 of 90% is as safe and clinically effective as 94%.5
The pathogenesis of respiratory failure in bronchiolitis is multifactorial,4,6 and NICE recommends that continuous positive airway pressure should be administered to children with impending respiratory failure.1 Airway suctioning is recommended in children with apnoea, respiratory distress or difficulty feeding because of secretions.1 Chest physiotherapy is recommended for those with a co-morbidity that affects their ability to clear secretions.
Despite its widespread use in paediatric practice, including on general paediatric wards, the NICE guideline does not discuss the use of heated humidified high-flow nasal cannula (HHHFNC) oxygen. Currently, insufficient evidence exists to show any benefit for use of HHHFNC oxygen.6–8
The current NICE guideline does not recommend the use of nebulised hypertonic saline. Published data from the UK Sabre trial and meta-analysis studies have found no evidence for their use, despite the Cochrane review in 2013, which suggested it may alter the course of the disease.9–11
Conclusions
Bronchiolitis is a lower respiratory infection of viral aetiology commonly affecting children less than one year of age during the winter months. Lacking curative treatment, the management remains supportive care. The NICE guideline on bronchiolitis published in 2015 aims to provide recommendations for the diagnosis, investigations and management of bronchiolitis.
Authors
Emma Caffrey Osvald BSc (Hons) BM MRCPCH
Astrid Lindgren’s Children’s Hospital, Karolinska University Hospital, Stockholm, Sweden
Jane R Clarke MRCP(UK) MD FRCPCH
Respiratory Department, Birmingham Children’s Hospital, Birmingham, UK
References
1 National Institute for Health and Care Excellence. Bronchiolitis in children. NG9. (accessed April 2017).
2 Scottish Intercollegiate Guidelines Network: Bronchiolitis in children. A national clinical guideline. 91. Edinburgh: Scottish Intercollegiate Guidelines Network, 2006.
3 Ralston SL et al. Clinical Practice Guideline: The diagnosis, management and prevention of bronchiolitis. Pediatrics 2014;134:e1474.
4 Meissner HC. Viral bronchiolitis in children. N Engl J Med 2016;7;374(1):62–72.
5 Rodriguez A et al. Oxygen saturation targets in infants with bronchiolitis (BIDS): a double-blind, randomised, equivalence trial. Lancet 2015;316:1041–8.
6 Sinha IP et al. CPAP and high-flow nasal cannula oxygen in bronchiolitis. CHEST J 2015;1;148(3):810–23.
7 Mayfield S et al. High-flow nasal cannula therapy for respiratory support in children. Cochrane Database Sys Rev 2014;3:CD009850.
8 Beggs S et al. High-flow nasalcannula therapy for infants with bronchiolitis. Cochrane Database Sys Rev 2014;1:CD009609.
9 Everard ML et al. SABRE: a multicentre randomised control trial of nebulised hypertonic saline in infants hospitalised with acute bronchiolitis. Thorax 2014;69:1105–12.
10 Everard M et al. Hypertonic saline (HS) for acute bronchiolitis: Systematic review and meta-analysis. Eur Resp J 2014;44(Suppl 58):P1226.
11 Zhang L et al. Nebulised hypertonic saline solution for acute bronchiolitis in infants. Cochrane Database Syst Rev 2013;7: CD006458.










