With high rates of venous thromboembolism (VTE) among those hospitalised with COVID-19, there is a need for early identification of those at risk.
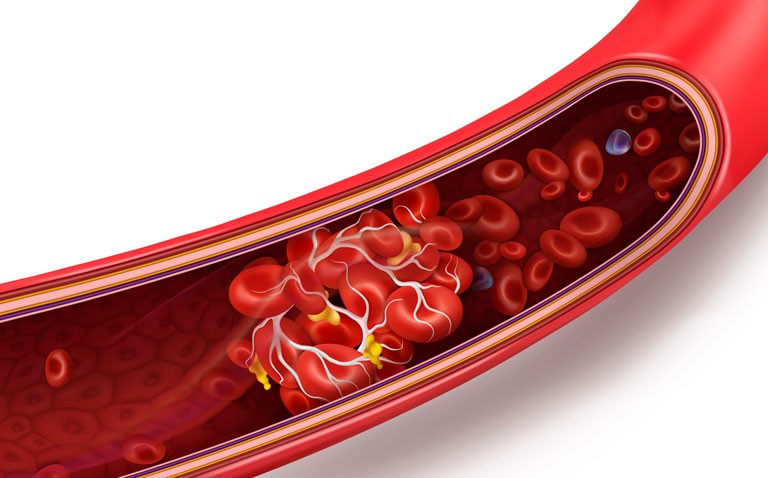
A venous thromboembolism (VTE) can occur either in deep veins (deep vein thrombosis, DVT) or in the pulmonary circulation (pulmonary embolism, PE).
Early in the COVID-19 pandemic it was recognised that coagulation abnormalities were present in those infected with the virus. In fact, one review of 36 studies found that the pooled incidence of VTE was 28%.
Consequently, it is important that clinicians are able to identify those at risk of symptomatic VTE to ensure appropriate management. Nevertheless, there is some lack of clarity over the most appropriate risk assessment tools.
With a lack of satisfactory prediction models, a team from Union Hospital, Tongji Medical College, Wuhan, China, decided to retrospectively explore not only the prevalence of VTE but potential risk factors among patients hospitalised with severe COVID-19.
The team conducted their study in 16 centres between January and March 2020 and collected information on patient’s demographics, clinical, laboratory and chest radiographs, treatment.
Symptomatic VTE was diagnosed based on both clinical manifestations, e.g. swelling and pain in the lower extremities, elevated D-dimer (> 0.5 microgram/ml) values and confirmation by imaging.
The team also used three clinical risk assessment models (Padua, the improve model and the Geneva model) for VTE on all patients.
In addition, they considered two additional models; one with “six-factors” (age, cancer, interval from COVID-19 onset to admission, fibrinogen concentration, D-dimer level of admission and if the D-dimer value increased > 1.5-fold) and a second, which the team termed the “Wuhan score”, based on only fibrinogen and D-dimer on admission and where the D-dimer value increased > 1.5-fold.
The team also examined a historical cohort of non-COVID-19 patients who developed VTE for comparative purposes.
Findings
A total of 2,779 COVID-19 patients were enrolled consisting of 1139 non-severe cases. The rates of VTE were 1.95% in those with severe COVID-19 compared to 0.87% in non-severe cases and 0.30% in non-COVID-19 patients.
After adjustment for age and gender, the odds ratio (OR) for developing symptomatic VTE was 5.94 (95% CI 3.91 – 10.09) in severe COVID-19 compared with non-COVID-19 patients. Moreover, this risk was also elevated in those with moderate severity COVID-19 (OR = 2.79).
When comparing symptomatic VTE models, the most significant factors were D-dimer increments > 1.5-fold (OR = 14.18), followed by D-dimer level on admission (OR = 1.33) and lower fibrinogen level upon admission (OR = 0.64).
The “Wuhan model” provided a sensitivity of 93% and a specificity of 71% for predicting symptomatic VTE compared with a sensitivity of 90.7% and specificity of 75.1% for the 6-factor model.
The authors concluded that their 3-factor score model which included three independent coagulation predictors for VTE, lower fibrinogen on admission, higher D-dimer on admission and increments in D-dimer while in hospital, showed good predictability compared to the 6-factor model and could be used to aid the early identification of COVID-19 patients who are at a high risk for symptomatic VTE.
Citation
Li JY et al. Clinical characteristics and risk factors for symptomatic venous thromboembolism in hospitalised COVID-19 patients: A multi-centre retrospective study. J Thromb Haemost 2021.