The overarching aim of NICE guideline NG161 is to enable cancer services to match the capacity for cancer treatment if services become limited during the pandemic.
Patient communication
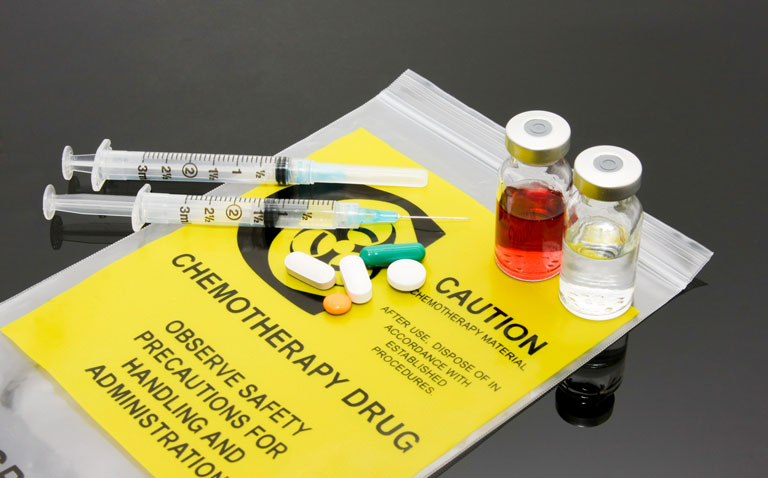
The initial focus of NG161 is to ensure that staff engage in effective communication with patients in receipt of systemic cancer treatments to support their mental wellbeing. It is particularly relevant for this patient group because both cancer and chemotherapy can weaken the immune system and thus lead to serious complications should someone become infected with COVID-19. NG161 therefore advises that healthcare staff minimise face-to-face contact with patients and to undertake more telephone or video consultations, especially for non-essential follow-up appointments and pre-treatment consultations. In addition, NG161 recommends the use of home delivery services for medicines, or alternatively drive-through medicine pick-up points as well as local services for blood tests wherever possible.
When patients do have to attend clinic appointments, NG161 recommends that they adhere to government suggested social distancing guidance and to attend appointments alone wherever possible. In addition, the guidance recommends that clinics carefully schedule visits and ask patients to remain in their car or with transport if possible until they receive a text message from the clinic confirming that they are ready to see them.
Patients with confirmed or suspected COVID-19
When a patient is identified as having COVID-19, the guidance recommends following appropriate infection prevention and control measures for healthcare workers. Specific guidance for COVID-19 has been recently produced and adapted from previous pandemic documents and is considered good practice in light of the current situation. The guidance contains information using personal protective equipment and states that patients are not infectious until the onset of symptoms (section 2.2) but that once an individual becomes symptomatic, they should be isolated in negative pressure rooms (section 6.2.1).
If a patient attends for an appointment and has symptoms suggestive of COVID19, NG161 suggests that healthcare staff follow the government advice which provide information on testing and isolating such patients. Although patients may exhibit symptoms of COVID-19, NG161 alerts clinicians to the possibility of alternative diagnoses such as neutropenic sepsis which according to an earlier NICE guideline is a potentially fatal complication of anticancer treatment. Another potential diagnosis is pneumonitis and NG161 makes reference to how both neutropenic sepsis and pneumonitis may be difficult to differentiate from COVID-19 on initial presentation. NG161 however, does advise that if patients have a fever but no respiratory symptoms, then neutropenic sepsis should be suspected. Because this can rapidly progress and is life-threatening, staff are advised to follow the neutropenic sepsis NICE guideline which recommends immediate referral of suspected cases to secondary or tertiary care and considering the condition as a medical emergency.
NG161 also discusses a course of action for patients who present at appointments with symptoms of COVID-19.
As with all the rapid new COVID-19 guidelines, NG161 recommends that healthcare workers who come into contact with dialysis patients follow the guidance on infection prevention and control.
NG161 also suggests that self-isolating staff should, if possible, undertake video or telephone consultations and attend virtual multidisciplinary team meetings. Self-isolating staff could also perform other roles including the identification of patients suitable for remote monitoring or those who are more vulnerable and in need of more support and undertake tasks such as data entry.
How to prioritise patient treatment
Due to the pandemic and the potential for resource limitations, NG161 defines a process for prioritisation of patients for systemic anticancer treatment. NG161 advises that prioritisation decisions (see table) are made by a multidisciplinary team and on an individual basis considering both the level of immunosuppression associated with the patient’s treatment and any relevant capacity issues. These decisions and the reasoning behind those decisions should be recorded and clearly communicated to the patient and their family or carers.
Modification to usual service provision
NG161 suggests that cancer teams seek to modify usual care in the wake of COVID-19 with a view to making best use of resources and reducing patient exposure to the virus. Suggested changes to usual care include:
• Delivery of different or fewer immunosuppressive anticancer regimes, delivery via a different location or if possible, alternative routes such as changing from intravenous to subcutaneous or oral (subject to agreement from commissioners)
• Using shorter regimes
• Decreasing the frequency of regimes for example, from four-weekly to six-weekly
• Providing repeat prescriptions of oral medicines or other at-home treatments so that patients do not need to attend the hospital/using home delivery of oral medicines where possible
• Deferring treatments that prevent long-term complications such as bone disease
• Using treatment breaks for treatments longer than six weeks.
Although treatment breaks were a suggested change in NG161, the guidance also notes that such breaks will not be applied during the COVID-19 pandemic. Nevertheless, where a break is needed, NG161 advises that clinicians document that the treatment break is due to COVID-19. Such breaks are likely to be approved provided that the clinician indicates that there is a reasonable chance that disease control can be achieved on re-starting therapy and that it should be reviewed after two or three cycles after re-starting.
NG161 advises that patients and their families should be fully informed of the reasons behind any treatment changes. The guideline also considers the possibility of re-training nurses who have previously undertaken relevant cancer training.
The guideline is available online and interested readers should check for any relevant updates.