Chronic obstructive pulmonary disease (COPD) is a disease characterised by chronic airflow limitation, and progressive and persistent respiratory symptoms.1 Today, COPD is the third largest cause of mortality worldwide, and its incidence increases gradually with smoking status.2 Emphysema is one of the subtypes of COPD, and its treatment with standard drugs is often difficult because of alveolar tissue damage, loss of elastic recoil, air trapping and hyperinflation.3 Pulmonary function tests in emphysema patients show increases in total lung capacity (TLC) and residual volume (RV) in addition to the classical COPD findings. Standard treatment regimens for COPD normally include smoking cessation, inhaler therapy, breathing exercises, nutritional support, as well as oxygen therapy and non-invasive ventilation in patients with severe emphysema.1 Unfortunately, these treatments do not always yield satisfactory results in patients with severe emphysema. In such patients, hyperinflation, local air trapping and intrathoracic compression are notable problems that result in increased breathing difficulty and place an additional burden on the respiratory muscles.
There are, however, other treatment options for patients with severe emphysema, such as lung volume reduction surgery, bullectomy and lung transplantation.4 Surgery is only suitable for selected patients due to intraoperative risks, postoperative complications, and increased mortality.5 In the last decade, endoscopic methods providing similar results to those of lung volume reduction surgery have been investigated, and minimally invasive methods have been developed.
The new and alternative treatment modalities, which are known as endoscopic lung volume reduction (ELVR) procedures, exert their effects through five main mechanisms: reduction of airway trapping; reduction of bronchoconstriction; improvement of elastic recoil; induction of local inflammatory reactions; and airway blockage.6 These ELVR procedures are endobronchial valve (EBV), coil, thermal vapour ablation, bio-lung volume reduction, targeted lung denervation, and airway bypass stent. An expert panel report on the EBV and coil methods has been published,7 and the other three procedures are currently in development. With increasing published evidence of effectiveness and safety, ELVR techniques have been available in the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines since 2017 and are recommended in a range of situations, from the presence of refractory conditions to maximal medical treatment regimens and pulmonary rehabilitation programs.1
Indications and patient selection
The major indication for treatment with ELVR methods is COPD of GOLD stage III or IV with severe emphysema. Values of patient forced expiratory volume in 1 second (FEV1) should be between 15% and 50% (15–45% for coil), and findings indicating the presence of hyperinflation (TLC >100%, RV >175%, RV/TLC ≥0.58) are required. Although there is no clear evidence, it is recommended by experts that these therapies should be avoided in patients with hypercapnia (PCO2 >55–60mmHg) and pulmonary hypertension (PAB > 50mmHg).7 Patient results for the 6-minute walk test (6MWT) should be in the range of 150–450m. Furthermore, these expensive treatments are not recommended for active smokers. To be considered for ELVR treatment, patients should have quit smoking at least two months prior; cessation of smoking six months before is most ideal (Table 1).
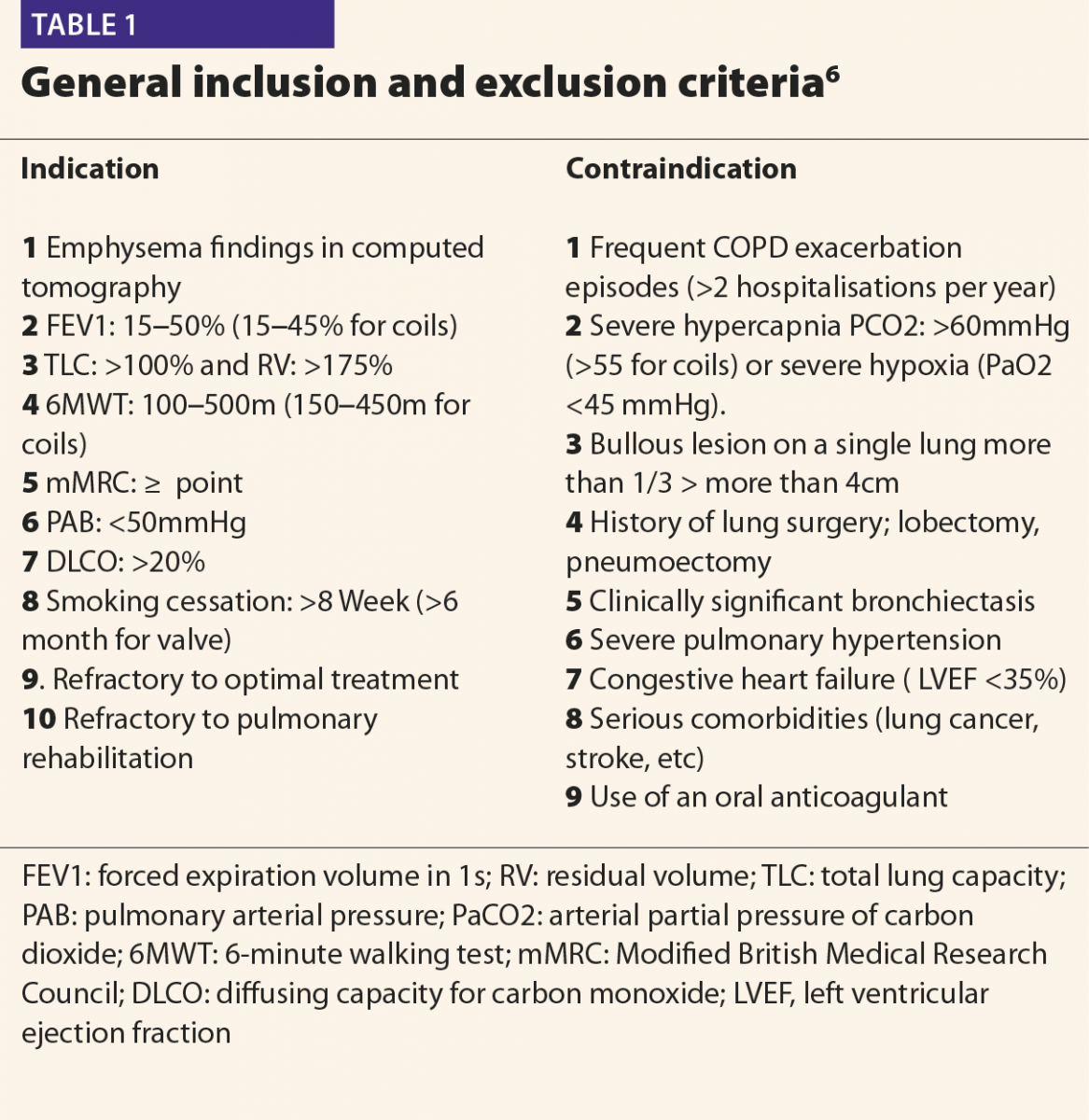
Contraindications
These treatments are not recommended for patients with clinically relevant bronchiectasis, lung cancer, bullous lesions greater than 4cm, history of prior lung surgery, severe hypoxia (PaO2 <45mmHg), hypercapnia (PCO2 >55–60), or in patients undergoing anticoagulation therapy.7 In addition, these treatments are not recommended in patients with impaired general status or in those who have comorbidities that might significantly affect survival. Other contraindications include unstable cardiovascular disease such as unstable arrhythmia, severe heart failure (left ventricular ejection fraction <35%), and stroke or myocardial infarction within the last six months.8 Although genetic α-1 antitrypsin deficiency has been accepted as a criterion for exclusion, discussion continues as to whether it should be considered as a contraindication.
Procedure
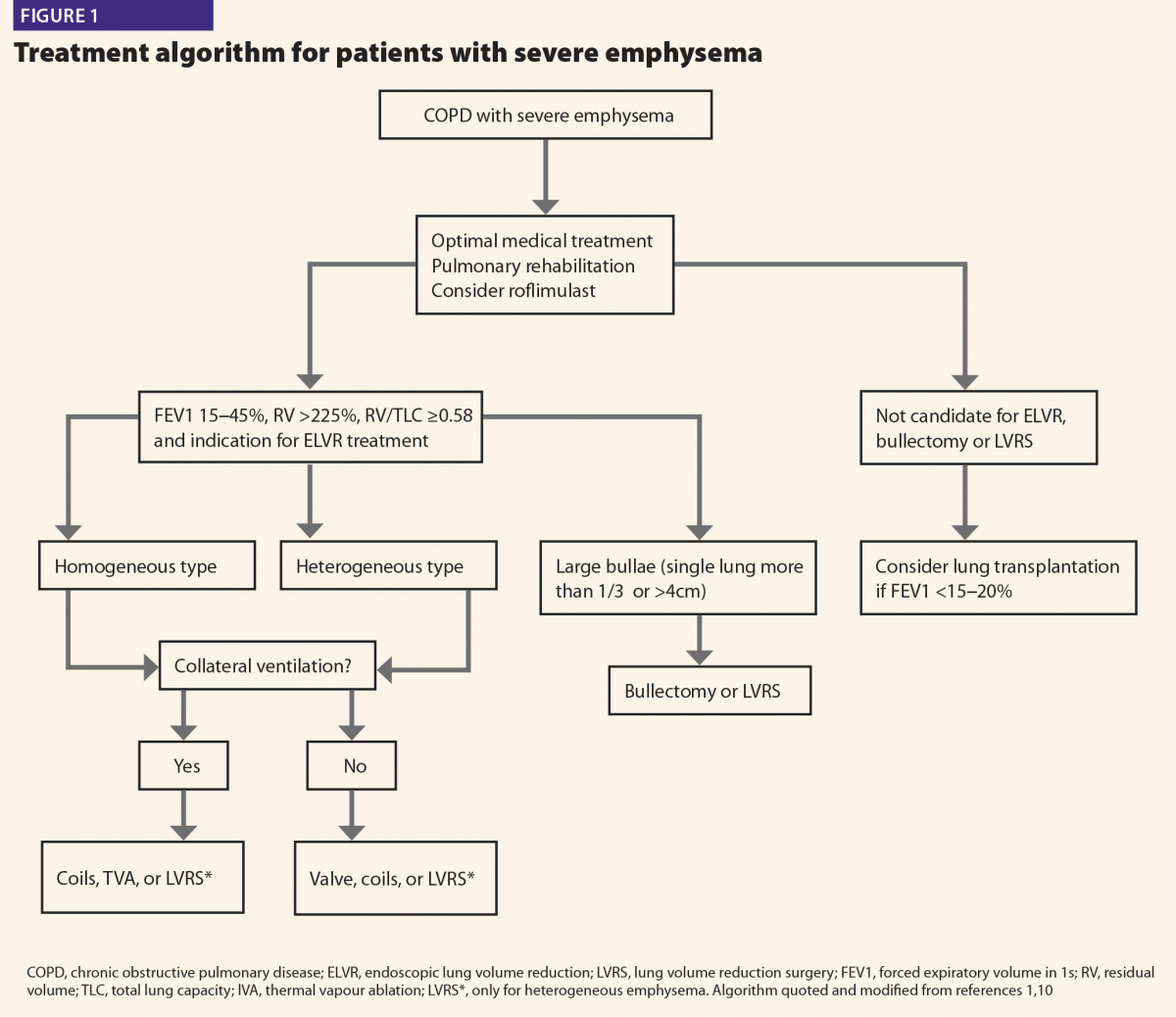
The most frequently used and most evidence-based ELVR methods are the valve and coil procedures. Although their mechanisms of action are different, these methods can be performed in patients with both heterogeneous and homogenous emphysema. The treatment algorithm for these methods is shown in Figure 1.1,9 The valves are fully reversible, and coils are partially reversible, but it is not possible to recycle all applied coils.10
Endobronchial valve implantation
The evaluation of collateral ventilation and the fissure completeness score (FCS) is very important prior to treatment. These evaluations are performed by qualitative computed tomography and via the Chartis system during bronchoscopy. If the FCS and collateral flow are above 95%, valve therapy can be applied directly. Measurement with the Chartis system is required when collateral flow is between 80% and 95%. However, alternative endoscopic methods and surgeries should be considered in patients with collateral flow scores below 80%.7 Under light sedation, endobronchial valves are placed into bronchoscopically targeted segmental bronchi. Atelectasis and volume-reducing effects are achieved after blocking the hyperinflated lung lobe. Targeted lobar volume reduction is the efficacy outcomes measure, which is considered to be positive when a reduction of 350ml is achieved.11
Endobronchial coil implantation
The coil procedure (PneumRx Inc, Mountain View, CA, USA) was developed for patients with heterogeneous and homogenous emphysema with interlobar collateral ventilation. The procedure is performed under general anaesthesia and fluoroscopy. Approximately 8 and 14 nitinol coils (average of 10) are placed in the targeted lobe using bronchoscopy. The length of the airway is measured by the guide wire during the procedure, and 100, 125, and 150mm coils are used in the procedure. Using the carrier catheter, the coil is advanced to the targeted bronchus, but it is recommended not to place it too close to the central vascular structures and pleura.12
By pulling the catheter, the coil returns to its original shape before it is loaded into the catheter, thus reducing lung volume. The same procedure is applied in the other lung within four to eight weeks. Following the procedure, patients are kept under observation for one to two days.
In order to obtain a good response, the patient must have healthy parenchymal tissue in the non-targeted lung areas.6–8
Benefits
In the studies conducted to date, EBV treatment resulted in an average increase in FEV1 values of 77.5ml (34.5–140.0ml), an increase in results of the 6MWT of 40.8m (9.3–91.0m), and an average decrease in RV values of 440ml (200–680ml).6 In addition, the following were observed: increased patient quality of life, a St George’s Respiratory Questionnaire (SGRQ) score decrease of 7.0 points, a modified Medical Research Council (mMRC) score decrease of 0.8 points, a BODE Index decrease of 1.2 points, and increased exercise tolerance.7
In a review of the coil procedure, it was reported that coil treatment resulted in an average increase in FEV1 values of 130ml (90–200ml), an increase in results for the 6MWT of 47.0m (14.6–84.0m), and an average decrease in RV values of 420ml (310–510ml).6 A significant increase in patient quality of life was also observed (SGRQ –12 points).7 Additionally, improvements in scores of anxiety and depression were recorded in this patient group.13 In a recent study, coil treatments were reported to cause improvements in blood gas parameters in patients with hypoxic or mild hypercapnic respiratory failure.14
Potential complications
Although ELVR therapies are minimally invasive procedures, they can lead to various complications due to the presence of COPD with severe emphysema. Pneumothorax (17.3%), valve migration (2.1%), pneumonia (1.7%), haemoptysis (1.9%), respiratory failure (1.4%), and exacerbations of COPD (0.9%) were reported in a recent study after application of EBV procedures.15 Pneumothoraces (86%) usually occur within the first 72 hours, indicating that patients should be hospitalised immediately for a minimum of 72 hours following the procedure.16
COPD exacerbation (41.0%) is the most frequent complication of coil procedures, followed by pneumonia (14.8%), and pneumothorax (5.7%).6 These complications may occur either immediately after the procedure or during follow-up. However, prophylactic antibiotics are frequently used by the bronchoscopist due to the high risk of COPD exacerbation and pneumonia. There is no general consensus on the best application of prophylactic antibiotics. Short-term steroid administration and stress ulcer prophylaxis are generally recommended to reduce the post-treatment acute inflammatory response.17
Use of anaesthesia during the procedure
The EBV procedure is generally performed with mild sedation, and the coil procedure is performed with general anaesthesia in the operating room. Although patients are generally able to undergo the procedure, it is sometimes necessary to postpone it because a patient might not be able to tolerate the stress of anaesthesia.10
Cost-effectiveness
ELVR treatment methods are expensive. Cost estimates following an analysis were: valve method ($12,943); coil method ($11,328); and volume reduction surgery ($2444).18 These calculations do not include the costs associated with the management of complications and hospitalisation. Depending on agreements with health care systems, the cost of the Chartis catheter and delivery system for a single procedure can vary from $9185 to $10,300. However, total costs for one year of coil treatments were approximately $53,521 and $5912 for follow-up patients.19 In a landmark study (REVOLENS), the initial cost of coil therapy seemed very high, therefore, large-scale studies are required to better determine this method’s long-term cost and efficacy.19
Conclusions
Increasing ELVR treatment modalities have expanded the treatment spectrum for COPD patients with severe emphysema. In a group of patients with severe COPD, who were potential lung transplant candidates, positive results were obtained with ELVR treatment, indicating that ELVR treatment can act as a bridge until the time of transplantation.20 The most important reason for increasing treatment efficacy is correct patient selection. Although the EBV and coil treatments are the most commonly used methods, there is emerging positive evidence for other methods, such as thermal vapour ablation, bio-lung volume reduction, and targeted lung denervation. Autologous blood application will be performed much more frequently in the near future due to its low cost and easy applicability.21 Most recently, a newly designed device known as the ‘reverser’, which is similar to the coil structure, was tested in pigs, and positive results were obtained.22 The creation of treatment algorithms, research on the long-term effects of these methods, prevention and control of complications, and appropriate development of these methods are the most important issues ahead.
References
1 Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2017. www.goldcopd.org/ (accessed July 2019).
2 Murray CJ, Lopez AD. Measuring the global burden of disease. N Engl J Med 2013;369:448–57.
3 Holloway RA, Donnelly LE. Immunopathogenesis of chronic obstructive pulmonary disease. Curr Opin Pulm Med 2013;19:95–102
4 Marchetti N, Criner GJ. Surgical approaches to treating emphysema: Lung volume reduction surgery, bullectomy, and lung transplantation. Semin Respir Crit Care Med 2015;36: 592–608.
5 Criner GJ et al. The National Emphysema Treatment Trial (NETT) Part II: Lessons learned about lung volume reduction surgery. Am J Respir Crit Care Med 2011;184:881–93.
6 Gülşen A. Bronchoscopic lung volume reduction: A 2018 review and update. Turk Thorac J 2018;19:141–9.
7 Herth FJF et al. Endoscopic lung volume reduction: An expert panel recommendation – Update 2019. Respiration 2019;97(6):548–57.
8 Slebos DJ et al. Endobronchial valves for endoscopic lung volume reduction: Best practice recommendations from Expert Panel on Endoscopic Lung Volume Reduction. Respiration 2017;93:138–50.
9 Gordon M, Duffy S, Criner GJ. Lung volume reduction surgery or bronchoscopic lung volume reduction: is there an algorithm for allocation? J Thorac Dis 2018;10:2816–23.
10 Gulsen A et al. Evaluation of bronchoscopic lung volume reduction coil treatment results in patients with severe emphysema. Clin Respir J 2017;11:585–92.
11 Welling JBA et al. Minimal important difference of target lobar volume reduction after endobronchial valve treatment for emphysema. Respirology 2018;23:306–10.
12 Slebos DJ et al. Endobronchial coils for endoscopic lung volume reduction: Best practice recommendations from an Expert Panel. Respiration 2018;96:1–11.
13 Bostancı K et al. Endobronchial coils in treatment of advanced emphysema: A single center experience. Turk Gogus Kalp Dama 2019;27:57–62.
14 Gülsen A. Effects of bronchoscopic lung volume reduction coil treatment on arterial blood gases. J Bronchology Interv Pulmonol 2019;26(2):90–5.
15 Fiorelli A et al. Complications related to endoscopic lung volume reduction for emphysema with endobronchial valves: results of a multicenter study. J Thorac Dis 2018;10:3315–25.
16 Gompelmann D et al. Clinical and radiological outcome following pneumothorax after endoscopic lung volume reduction with valves. Int J Chron Obstruct Pulmon Dis 2016;11:3093–9.
17 Herth FJ et al. Assessment of a novel lung sealant for performing endoscopic volume reduction therapy in patients with advanced emphysema. Expert Rev Med Devices 2011;8:307–12.
18 Metin B et al. A single-center comparison of the cost analyses of different volume reduction-therapy methods in the treatment of emphysema. Cukurova Med J 2017;42:721–79.
19 Deslée G et al; REVOLENS Study Group. Lung volume reduction coil treatment vs usual care in patients with severe emphysema: The REVOLENS Randomized Clinical Trial. JAMA 2016;315:175–84.
20 Gulsen A. Importance of bronchoscopic lung volume reduction coil therapy in potential candidates for lung transplantation. Biosci Trends 2018;12:395–402.
21 Bakeer M et al. Low cost biological lung volume reduction therapy for advanced emphysema. Int J Chron Obstruct Pulmon Dis 2016;11:1793–800.
22 Hu Y et al. A new-designed lung-bending device for bronchoscopic lung volume reduction of severe emphysema: A feasibility study in pigs. Respiration 2019;97(5):444–50