The presence of an abnormal chest X-ray led to an increased diagnosis of intrathoracic malignancies including non-small cell lung cancer.
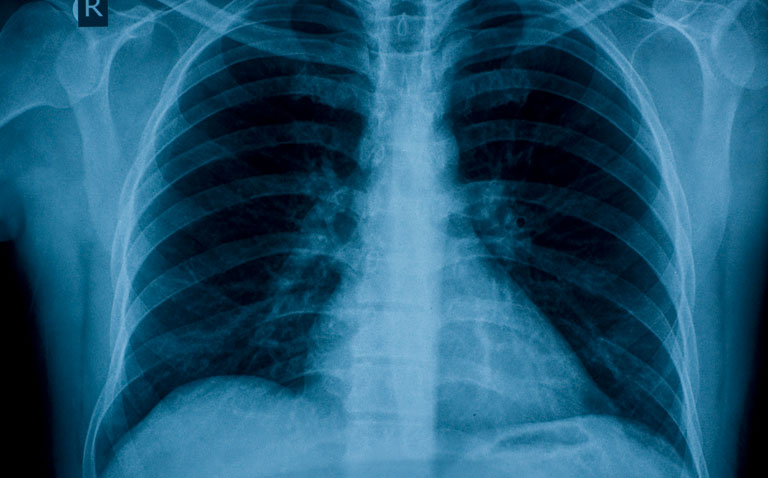
An abnormal chest x-ray can help to triage patients who might have lung cancer although the evidence base to support this role is incomplete. However, many studies in the past have failed to adequately define a positive chest x-ray and because of this, a team from the Department of Clinical Radiology, St James Hospital, Leeds, UK, decided to retrospectively examine a cohort of consecutive “self-request” chest x-rays collected as part of the National Awareness and Early Diagnosis Initiative (NAEDI) in the UK. The aim of their study was to establish the accuracy of the chest x-ray in the investigation of malignancy amongst symptomatic adults over the age of 50 years.
For the purposes of the study, the team defined as positive, an abnormal chest x-ray that resulted in the further investigation with computed tomography (CT). Furthermore, because the term thoracic malignancy encompasses a range of tumours, they focused on evaluating the accuracy of the chest x-rays in the detection of non-small cell carcinomas (NSCLC). As part of the NAEDI, patients completed a questionnaire and were able to obtain a chest x-ray without the need for a referral on a walk-in basis to the radiology department, provided that they met the eligibility criteria (based on the questionnaire results) which were symptoms lasting longer than three weeks (cough, haemoptysis, shortness of breath, chest pain, change in voice or loss of weight). At the time of the study, a history of smoking was not a requirement. The main outcomes reported were the sensitivity and specificity for NSCLC and all primary intrathoracic malignancies within a one and two year period. The team determined the sensitivity as the number of cancer diagnoses identified on the basis of a positive CXR divided by the total number of cancers observed. Specificity was defined as the number of negative CXRs divided by the total number of CXRs in those without cancer.
Findings
A total of 8,948 questionnaires were evaluated with 496 (5%) abnormal chest x-rays (i.e., positive) and which resulted in a diagnosis of 133 patients with a primary intrathoracic malignancy in the first year and 168 after 2 years, including 105 and 133 NSCLC in the first and second year respectively.
The sensitivity for NSCLC identified within 1-year was 76.2% (CI 68.0–84.3) and the specificity 95.3% (CI 94.9–95.7). Within 2-years, the corresponding sensitivity was 60.2% (CI 51.8–68.5) and specificity 95.3% (CI 94.8–95.7). Although smoking was excluded from the inclusion criteria, 23% of the cohort were current smokers and 44% ex-smokers. The corresponding 1-year sensitivity for the detection of NSCLC in smokers was 83.3% (95% CI 67.1 – 92.4) and 71.6% (95% CI 57.7 – 82.3) for ex-smokers. The corresponding specificities were 94.2% (current smokers) and 95.4% (ex-smokers).
The authors noted that while a negative chest x-ray does not exclude a diagnosis of malignancy, the baseline risk of lung cancer in the current cohort was 1.9% and that a negative x-ray would reduce this risk to 0.8%. They concluded that a positive chest x-ray is strongly predictive for the presence of malignancy but added that a negative result does not conclusively exclude the diagnosis but allows for an estimation of the risk of malignancy.
Citation
Bhartia BSK et al. A prospective cohort evaluation of the sensitivity and specificity of the chest X-ray for the detection of lung cancer in symptomatic adults. Eur J Radiol 2021