Do-it-yourself (DIY) human papillomavirus (HPV) tests could be a ‘game changer’, enabling a million more women in England to participate in cervical screening over the next three years, a new study has suggested.
Researchers from King’s College London (KCL) concluded that offering self-sampling kits to women who were at least six months overdue for cervical screening could result in 400,000 more women being screened for cervical cancer each year.
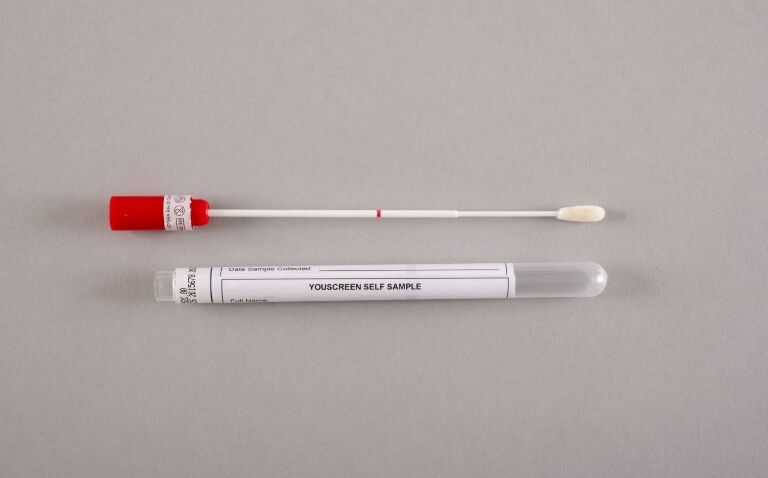
Supported by Cancer Research UK, the YouScreen trial is the largest self-sampling trial conducted for cervical cancer. It offers women the chance to screen themselves at their GP surgery or in the privacy of their own home.
The trial’s results, published in the journal eClinicalMedicine, highlight a simple and effective way to increase the number of people taking cervical smear tests.
Cervical cancer is highly preventable by screening and treating pre-cancer. However, cervical screening participation has been falling in England for over two decades and women who do not regularly attend screening appointments are at the highest risk of developing cervical cancer. Almost a third of eligible women are not being routinely screened; in some parts of London, this is as high as 50%.
Self-sampling has been shown in previous studies to be as effective in detecting HPV as smear tests taken by healthcare staff and can remove some barriers for women who would like to be tested but are put off by the standard cervical smear process.
In partnership with the NHS Cervical Screening Programme, the researchers tested the DIY kits across 133 GP surgeries in North Central and North East London, offering over 27,000 unscreened and under-screened women HPV self-sampling kits between January and November 2021.
People in the trial used a vaginal swab to take their sample either at home or at their GP practice. Samples taken at home could be posted for free directly to the laboratory for testing. If HPV was detected in any samples, a follow-up test was required.
The self-sampling intervention resulted in a 22% increase in non-attenders screened per month, with over 8,000 people using and returning the kits for testing. The women who tested were all between 25 and 64 years of age, with 64% being from ethnic minority groups and 60% from deprived populations. Women were more likely to use the self-sampling kits when they were offered at their GP practice. Some 56% of women self-sampled at their GP surgery, compared to 13% when the kit was sent directly to their home.
Lead investigator Dr Anita Lim, a senior epidemiologist at KCL, said: ‘Self-sampling has been hailed as a game-changer for cervical screening, and we now have evidence in a UK population to show that it is.’
She added: ‘It is crucial that we make cervical screening easier by introducing innovations like self-sampling, alongside the current cervical screening programme, to help protect more people from this highly preventable cancer. Self-sampling can do this by offering people choice and convenience.’
The trial showed that the DIY test is popular with both women and GP practices, and the self-sampling kits enabled screening for a wider population.
Dr Lim added: ‘It’s encouraging that we received self-samples from groups that have been historically underserved, including people from deprived and ethnic minority backgrounds, LGBTQI+, people with learning disabilities and victims of sexual violence.’
Miss Alexandra Lawrence, from the North East London Cancer Alliance and consultant gynaecological oncologist at St Bartholomew’s and the Royal London Hospital, said: ‘Self sampling was hugely popular with women and in primary care during the YouScreen study. Introducing this option will help to address the low uptake of cervical screening in our area of London. Early detection is so important for all cancers and cervical screening enables HPV-related changes on the cervix to be treated before cancer even develops.‘
The NHS is now set to work with the UK National Screening Committee to consider the feasibility of rolling this out more widely across England.
This comes as the latest figures show that of the 11 million 25-49-year-olds eligible for cervical screening, only 65.8% took up invitation and were screened within the recommended time as of December 2023. This rose to 74.1% of those aged between 50 and 64.
Steve Russell, chief delivery officer and national director for vaccinations and screening for NHS England, said: ‘We have set an ambitious target of eliminating cervical cancer within the next two decades – one of the few countries in the world who have committed to this – and we are doing everything we can to achieve our ambition by making it as easy as possible to make appointments, and continuing to send invites and reminders to all eligible women.‘
Evidence has suggested that cancer screening for breast, colorectal and cervical cancers significantly reduced across the world during the Covid-19 pandemic.
But even in 2019, a UK study found that only a third of women take up all offered cancer screenings.
Image credit: YouScreen
A version of this article was originally published by our sister publication Nursing in Practice.