The recent label extension of an enzymatic debridement treatment could mark a paradigm shift for paediatric burns. Professor Stan Monstrey, former head of the Plastic Surgery Clinic and Burn Center at Ghent University Hospital, speaks to Katherine Price about how treatment has evolved and opportunities yet to be realised.
Nearly a third of all burn patients admitted for treatment in Europe are children, who often sustain major injuries that require critical intervention and can be more susceptible to scarring due to thinner skin and overreactive scar tissue formation.
Scars are likely to have a lasting and potentially devastating impact in childhood – a critical period for establishing and improving physique, personality, social contacts and values.
As such, following significant improvements in the morbidity and mortality associated with burn injuries, the focus of burn care has shifted from only healing and survival to quality of survival. That is to say scar prevention, achieving the best functional and aesthetic outcome and supporting wellbeing.
‘Scarring is [an] inflammatory process which is an overreaction of the body to try to heal the wound. Especially for children, children do have more reaction capacity, and they react with more inflammation,’ says Professor Stan Monstrey, a leading European plastic surgeon, burn specialist and former secretary general and president of the European Association of Plastic Surgeons, who has nearly 40 years’ experience treating burn patients.
’If you compare a 13-year-old girl with a 73-year-old woman, the child will be much more at risk of developing hypertrophic scars and contractures,’ he adds.
Developments in assessing wound depth
Paediatric burn management has come a long way in the last decade, with Professor Monstrey among those at the forefront of these developments, particularly due to the introduction of laser Doppler imaging (LDI).
The accuracy of LDI in determining healing potential has been a real gamechanger in burn wound treatment, he says.
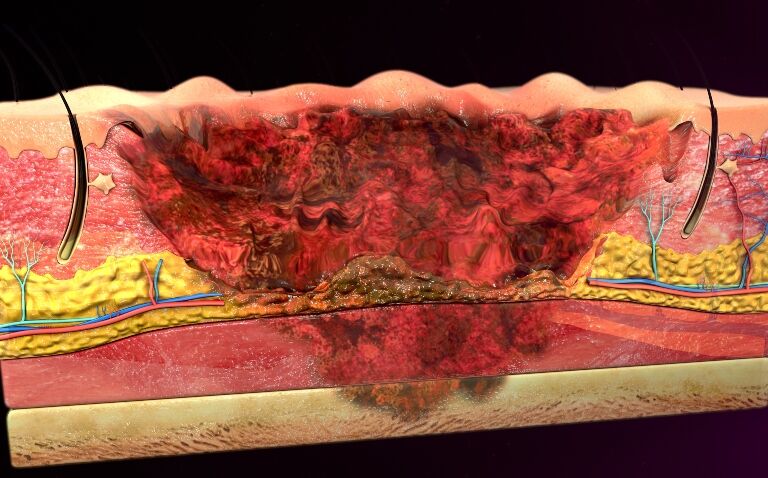
Burn depth is one of the most important factors when deciding whether to treat a burn as superficial, which will heal by itself and can be treated conservatively, or deep, which need to be treated surgically.
This cannot always be accurately assessed visually by clinicians, especially immediately after an injury. There is a clinical burn depth assessment accuracy of 50-75% and, Professor Monstrey says, ‘approximately 50% of wounds fall into the category of intermediate-depth burns’.
LDI measures blood flow and therefore the wound healing potential and depth of a burn, which can help clinicians to assess the risk of hypertrophic scars, and therefore guide their treatment decisions based on the aesthetic and functional outcome possibilities.
The scans map blood flow with colour: blue and green indicate low perfusion of injury tissue (deep burn), yellow a moderate perfusion (between superficial and deep burn), and red a higher perfusion of injured tissue (superficial burn).
Professor Monstrey points out that LDI has helped clinicians assess two to five days following injury if the wound is going to heal within two weeks, between two and three weeks, or longer than three weeks, depending on its depth – and therefore whether surgery is necessary.
Enzymatic debridement
Use of an enzymatic debriding agent is an effective way to remove eschar from burn wounds, reducing inflammation and incidence of hypertrophic scarring. Currently, NexoBrid is the only effective enzymatic debriding agent available.
Based on the results of several evidence-based studies, the Belgian National Institute for Health and Disability Insurance granted a final reimbursement for Nexobrid treatment in adults – an approach Professor Monstrey hopes more countries will adopt not only for adults but paediatric patients, too.
He acknowledges there are logistical, workforce and financial hurdles to the expansion and funding of such treatment, however. ‘It is painful, which means you need the collaboration of an anaesthesiologist,’ he points out.
Although the treatment has been focused on deep wounds, some patients with LDI yellow to green burn wounds, especially in the younger population, still develop hypertrophic scars with conservative treatment – ‘about 20%’, Professor Monstrey estimates.
As a result, the next step for Ghent University is to investigate if yellow wounds could and should also be treated with enzymatic debridement.
The Committee for Medicinal Products for Human Use (CHMP) recently adopted a positive opinion recommending a paediatric label extension for NexoBrid, an enzymatic debridement treatment for deep partial- and full-thickness thermal burns containing concentrate of proteolytic enzymes enriched in bromelain.
The active substance is a mixture of enzymes extracted from the stem of the pineapple plant, which act as a debriding agent to dissolve eschar without harming surrounding viable tissue in most cases.
The label extension was based on the results of a global Phase 3 trial that demonstrated a significant reduction in eschar removal time, incidence of surgical excision and the need for autograft in deep partial burns, as well as a favorable trend in the reduction of blood loss during the eschar removal process. In addition, the study confirmed NexoBrid to be well-tolerated in all age groups.
Since introducing the treatment at Ghent University Hospital’s Burn Center around eight years ago, ‘about half of the cases healed by themselves, so we could avoid an operation’, says Professor Monstrey.
‘Since we’ve had NexoBrid, not one patient has needed an escharotomy because it dissolves the eschar and allows the tissue to swell to what degree is necessary,’ he adds.
With the paediatric label extension, it is hoped that this same success will be extended to children as well, offering them improved quality of survival.
Unmet needs in burn care
While effective enzymatic debridement treatments are a very welcome addition to a clinician’s arsenal in the treatment of paediatric burns, Professor Monstrey has been disappointed by the lack of success in developing dermal substitutes for full thickness burns.
‘When I was a resident there was a lot of research already into dermal substitutes, so what I had in mind was that for extensive burns, we would be able to provide a good quality dermal substitute and then put a cover on that with cultured epidermal cells, which could mean a huge extension of complete skin recovery,’ he explains.
‘To my severe disappointment, the ideal dermal substitute has not been found yet.’
And although infection rates have improved over the years, ‘we still can’t say that this problem is completely gone’, he adds, with extensive burns continuing to present a challenge to clinicians.
However, Professor Monstrey is positive about the paradigm shifts and developments in aftercare and scar treatment over the last 15-20 years that have improved patient quality of survival.
‘We have been really focusing on the aftercare, which we think is as essential as all the rest,’ he says. This includes a whole host of products and treatments such as compression garments, silicone application, moisturisers, the list goes on.
Professor Monstrey concludes: ‘The paradigm shift is from survival to quality of survival – how can this patient end up with the least scars and the optimal aesthetic and functional outcome? This is in our minds right from the start.’