An analysis of breast cancer trial data suggests that tumour size and use of tamoxifen are both associated with greater long-term survival.
Breast cancer is the most common cancer in women worldwide and in 2020, there were 2.2 million cases and nearly 685,000 deaths. Breast cancer is a heterogenous disease with various types and different sensitivities to treatment, e.g., oestrogen receptor (ER) positive, progesterone receptor (PR) positive and hormone receptor (HR) negative. Among those with ER positive tumours, treatment with adjunctive therapy such as tamoxifen for five years is recommended. Nevertheless, even after treatment with tamoxifen, breast cancer can return over the intervening years, metastasise and lead to death. The use of clinical breast cancer markers such as tumour size or grade can be used to provide estimates of survival for up to 10 years and both increased tumour size and grade are associated with a reduced short-term survival. However, what is far less clear, is whether any of these markers are associated with longer term survival.
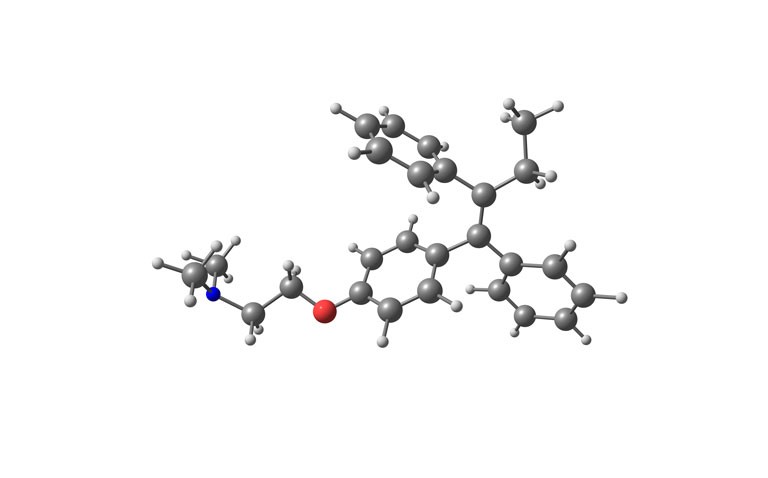
Given that both ER-positive and ERBB2-negative (i.e., HER2) disease are associated with a continuous risk of recurrent disease after the primary diagnosis, a team from the Department of Oncology and Pathology, Karolinska Institute, Stockholm, Sweden, sought to determine whether both clinically used markers and treatment with tamoxifen were associated with long-term survival in patients with breast cancer. The team turned to data from the Stockholm tamoxifen (STO-3) trial, which enrolled postmenopausal women with lymph-node negative breast cancer and tumours less than 30mm in diameter, between 1976 and 1990 and who were randomised to tamoxifen 40mg daily or no endocrine therapy. In 1983, women with no recurrence after 2 years on tamoxifen, were given the drug for a further 3 years. The team undertook an analysis of tissue samples that were available from patients in the study. The tumour grade (1 to 3) had been assessed in 2014 by a pathologist and tumour size was categorised as T1a/b if 10mm or less, T1c if 11–20mm and T2 if larger than 20mm. All patients had a unique national registration number and which was linked with a cancer registry, allowing the team to obtain long-term follow-up data after 25 years.
Findings
The sample contained 565 postmenopausal women with a mean age of 62 years. Just over half (52.2%) of tumours were graded as T1c and nearly a third (30%), T1a/b. Patients with T1a/b tumours had the best long-term survival (88%) compared to those with T1c tumours (76%) or T2 tumours (63%). Similarly, the highest level of survival (81%) occurred in those with grade 1 tumours compared with grade 3 tumours (65%). Using this data, the team estimated a 69% reduced risk of disease recurrence for those with T1a/b sized tumours (hazard ratio, HR = 0.31, 95% CI 0.17–55). In terms of treatment, those given tamoxifen with grade 1–2 tumours also experienced a significantly reduced risk of disease recurrence (HR = 0.24, 95% CI 0.07 – 0.82) compared with those who did receive the drug. However, use of tamoxifen also produced a significant survival benefit in those with T2 tumours (HR = 0.34).
The authors concluded that tumour size, followed by grade and use of tamoxifen were independently associated with long-term survival in breast cancer.
Citation
Dar H et al. Assessment of 25-Year Survival of Women with Oestrogen Receptor–Positive/ERBB2-Negative Breast Cancer Treated with and Without Tamoxifen Therapy. A Secondary Analysis of Data from the Stockholm Tamoxifen Randomised Clinical Trial. JAMA Netw Open 2021.