A first-in-class drug derived from olive oil has shown early promise in patients with an advanced form of brain cancer in a new trial led by The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research.
Idroxioleic acid (2-OHOA), is a synthetic lipid derived from olive oil, comes in a small sachet and is taken with water three times a day.
It works by regulating the cell membrane composition by both direct incorporation into the lipid bilayer and regulation of important lipid metabolism enzymes, such as sphingomyelin synthase 1 (SMS-1), stearyl CoA desaturase 1 (SCD1), phospholipases 1 and 2 (PLA1/2).
As such, 2-OHOA blocks crucial growth signals that drive cancer and can prevent it from growing or spreading, offering a new treatment for difficult-to-treat glioblastoma.
The trial, supported by the National Institute of Health, is the first time this drug has been studied to treat glioblastoma. The findings are published in the British Journal of Cancer and highlight the urgent need to accelerate the development of 2-OHOA.
Glioblastoma shows ‘exceptional response’
The open-label, non-randomised trial aimed to evaluate the safety, tolerability, pharmacokinetics, pharmacodynamics and anti-tumour activity of daily oral treatment with 2-OHOA monotherapy.
A dose-escalation phase using a standard 3 + 3 design was performed to determine safety and tolerability. This was followed by two expansion cohorts at the maximum tolerated dose to determine the recommended Phase-2 dose.
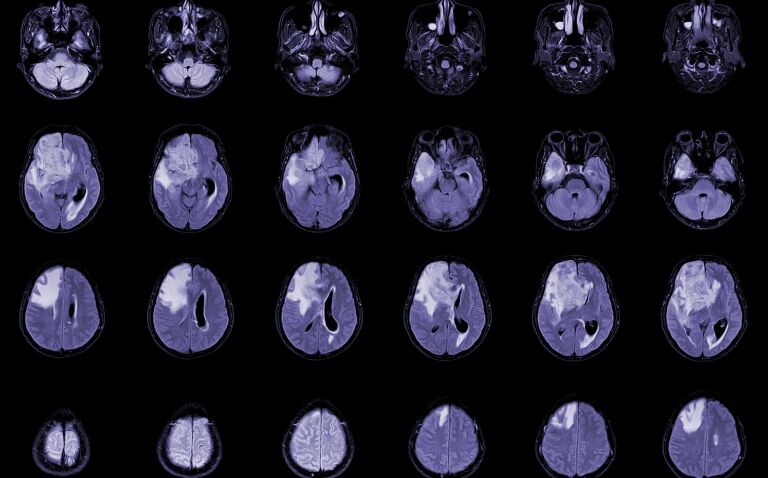
The researchers recruited 54 patients with recurrent glioblastoma and other advanced solid tumours to the trial. Of these, 21 patients with glioblastoma had a radiological assessment at baseline and at least one post-baseline time point and were therefore included in tumour response analysis.
Five patients (24%) treated across the dose escalation and expansion saw clinical benefit according to the response assessment in neuro-oncology (RANO) criteria (RANO CR, PR and SD >6 cycles). One patient was still alive after three years, which the researchers noted was an ‘exceptional response’.
Indeed, as Dr Juanita Lopez, a study lead and consultant medical oncologist at The Royal Marsden NHS Foundation Trust and reader at The Institute of Cancer Research, London, said: ‘Glioblastoma is an incredibly difficult disease to treat and, unfortunately, patients with advanced disease have very poor outcomes, often living for just a year after their diagnosis.’
She added: ‘There hasn’t been an effective new treatment for this patient group in nearly two decades, so drug development urgently needs to be accelerated.’
Often, patients with brain cancer do not have the opportunity to participate in early-phase trials, but the researchers hope this work will ensure their inclusion in the subsequent phases of the trial.
Commenting on ongoing trials, Dr Lopez said: ‘By including glioblastoma patients in this study, we were able to more quickly show early and hopeful results, supporting their inclusion in the Phase 2b/3 trial. We’re very much looking forward to results from ongoing trials and hope this treatment eventually becomes widely available.’
A phase 3 trial of the drug 2-OHOA is being launched by The Royal Marsden NHS Foundation, which is recruiting more than 200 newly diagnosed glioblastoma patients.
Other research is also underway looking at the combination of the arginine-depleting agent pegargiminase and chemotherapy in patients who have glioblastoma multiforme or sarcoma and other cancers dependent on arginine.