CAR T cells made in 24 hours are both effective and have an acceptable safety profile in patients with acute lymphoblastic leukaemia according to a first-in-human study
CAR T cells (CTC) which can be manufactured in a single day have been shown to be effective and with an acceptable safety profile, for the treatment of patients with relapsed or refractory B cell acute lymphoblastic leukaemia according to a first-in-human clinical study by a group of Chinese researchers.
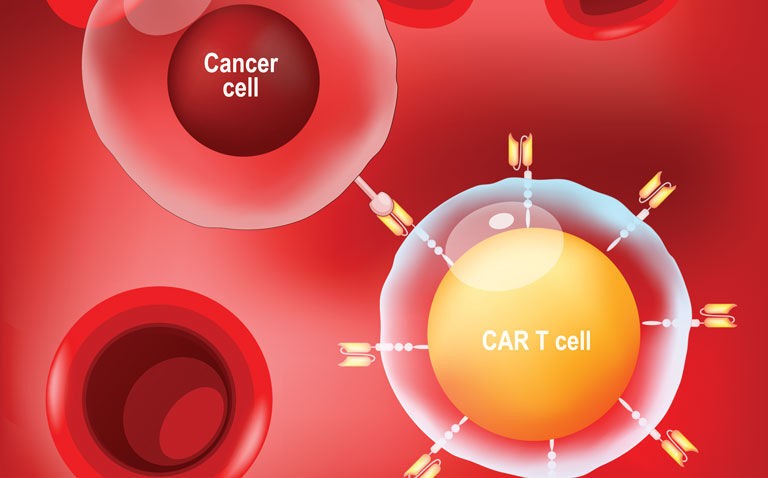
In CTC therapy, the patient’s own T cells are genetically engineered and then re-infused in an effort to eliminate their tumour cells. The T cells contain an extracellular ligand binding domain which is able to recognise antigens displayed on the surface of tumour cells (normally CD19).
Nevertheless, as more clinical trials have been undertaken, it has become evident that 30-60% patients relapse after treatment, probably due to persistence of CAR T-cells and escape or down-regulation of CD19 antigen. A further problem is that the T-cell engineering process can take 9 to 14 days and up to four weeks before infusion back into the patient.
For the present study, the Chinese team developed a type of CAR T cells that were manufactured using a novel process completed in 24 hours. The final product CTC product, GC007F, was tested in patients with relapsed or refractory B cell acute lymphoblastic leukaemia and for comparative purposes, the researchers also manufactured CTCs by conventional methods.
CAR T cells and patient outcomes
A total of 21 patients with CD19+ relapsed or refractory B cell acute lymphoblastic leukaemia were enrolled and given a single infusion of GC007F cells although only 18 were included in the final analysis after the others withdrew due to adverse effects. The median peak of CAR T cells was on day 10 and the median persistence was 56 days. The GC007F cells also showed better proliferation and tumour killing than conventional CTCs.
After 28 days, all patients had achieved complete remission (CR), with 17 achieving CR and maintaining minimal residual disease negative, MRD (i.e., no disease was detected after treatment) after 3 months. Additionally, at 6 months, 16 patients maintained CR with 14 maintaining MRD negative and the longest duration at the time of writing was 29 months without the need for transplant.
In terms of safety, 95.2% (n = 20) of patients experienced cytokine release syndrome (a recognised adverse effect) and which was greater than grade 3 (i.e., severe) in 52.4% (11) of patients. Neurotoxicity developed in 6 patients and was greater than grade 3 severity in 3 patients.
Overall, eight patients underwent allogeneic haematopoietic stem cell transplantation after GC007F treatment.
The authors concluded that these preliminary data suggested that their next day GC007F cells appeared to be effective and with a manageable toxicity profile.
Citation
Zhang C et al. Novel CD19 chimeric antigen receptor T cells manufactured next-day for acute lymphoblastic leukemia Blood Cancer J 2022