A significant five-year overall survival rate has been observed with the use of neoadjuvant nivolumab in resectable non-small cell lung cancer.
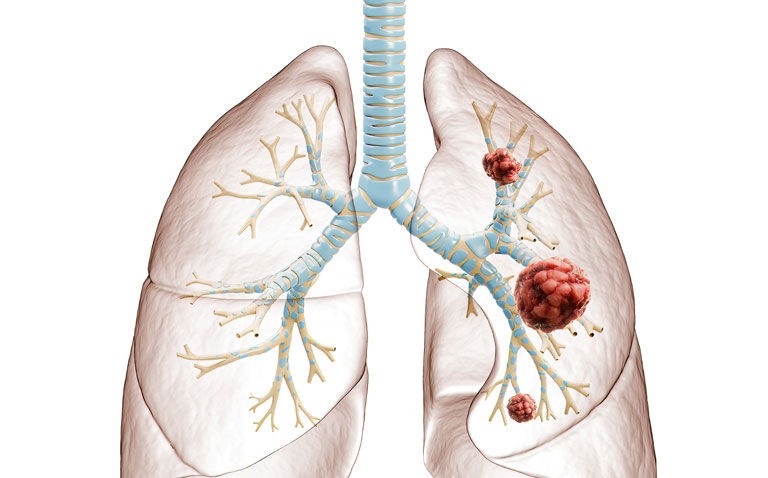
In a 2018 global study, lung cancer was found to be the most commonly diagnosed cancer (11.6% of all cases) as well as the leading cause of cancer deaths. The most common form of lung cancer is non-small cell lung cancer (NSCLC) which accounts for around 80-85% of all cancers. The use of programmed death 1 (PD-1) protein inhibitors as a treatment for patients with advanced NSCLC have been shown to produce a durable response and encouraging survival rates. Until recently, the value of PD-1 blockage in patients with resectable NSCLC has been unclear. However, in a 2018 trial it was found that two preoperative doses of nivolumab in adults who had early, i.e. stage I, II of IIIA, surgically resectable NSCLC, did not cause a delay to surgery and was able to induce a major pathological response in nearly half (45%) of resected tumours. While these were impressive, there was uncertainty over the longer term outcome of such patients.
In the current study, a team from Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, Baltimore, Maryland, US, provided the longest known follow-up study of patients given neoadjuvant nivolumab therapy with any type of cancer. The patient cohort was derived from the team’s earlier 2018 trial described above. Eligible participants received two doses of nivolumab (3mg/kg bodyweight) every two weeks with surgical resection planned for roughly four weeks after the first dose. In this follow-up, the researchers examined exploratory endpoints such as recurrence-free survival (RFS) and overall survival (OS) from the date of the patient’s surgery. They also considered the proportion achieving a major pathological response (MPR).
Five-year overall survival and neoadjuvant nivolumab
A total of 20 patients were included and followed for a median of 63 months. The five-year RFS rate was 60% and the OS 80%. In addition, the researchers reported that the use of nivolumab was associated with few side effects and did not delay surgery.
At the time the analysis was undertaken, the hazard ratio (HR) for the presence of a MPR, though not significant, was in the direction of improved RFS (HR = 0.61, 95% CI 0.15 – 2.44). In fact, at the five-year follow-up, eight of nine patients with a MRP were alive and free of disease. In contrast six of the 11 patients without MRP at a tumour relapse, three of whom died.
The authors concluded that five years, the clinical outcomes associated with neoadjuvant therapy were comparatively favourable to the earlier observed response. They added that while there was a trend towards improved RFS, it was difficult to draw any firm conclusions due to the small sample size.
Citation
Rosner S et al. Five-Year Clinical Outcomes after Neoadjuvant Nivolumab in Resectable Non-Small Cell Lung Cancer. Clin Cancer Res 2023