Ivosidenib added to azacitidine therapy produces a three-fold higher overall survival in older patients with acute myeloid leukaemia
Addition of ivosidenib to azacitidine therapy in older patients with acute myeloid leukaemia (AML) improved overall survival, event-free survival and clinical response according to results presented at the ASH 2021 conference by researchers from Hospital Universitari i Politècnic La Fe, Valencia, Spain.
The results were derived from the AGILE trial which is a global, Phase III, multicentre, double-blind, randomised, placebo-controlled clinical trial to evaluate the efficacy and safety of Ivosidenib (IVO) and azacitidine (AZA) compared to placebo and azacitidine in adult patients with previously untreated isocitrate dehydrogenase 1 mutations (IDH1m) AML and who are considered appropriate candidates for non-intensive therapy.
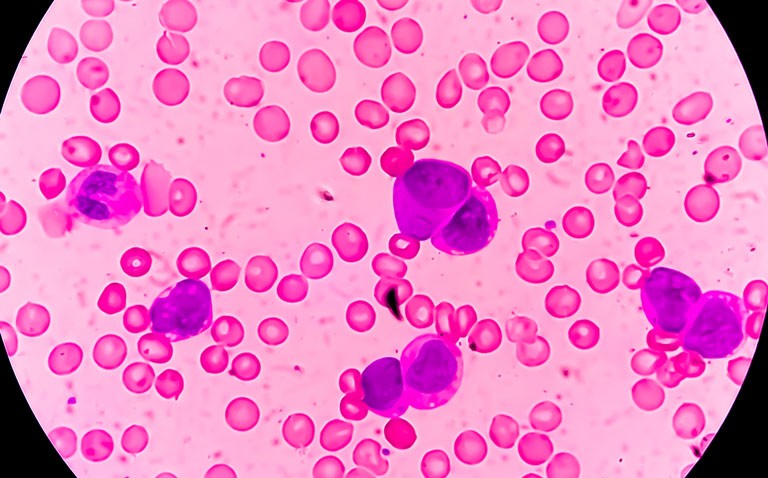
Somatic mutations in IDH1 are present in between 6 and 10% of patients with AML and Ivosidenib, is an oral, potent inhibitor of the mutant IDH1 (mIDH1) enzyme and approved by the FDA for adults with relapsed/refractory mIDH1 AML and those with newly diagnosed mIDH1 AML who are ≥ 75 years or have comorbidities that preclude use of intensive induction chemotherapy. Data from an earlier phase 1b study of 23 patients with newly diagnosed mIDH1 AML showed a favourable safety profile and encouraging clinical activity of the ivosidenib + azacitidine combination.
For the present study, the Spanish team randomised patients 1:1 to IVO 500 mg once daily + AZA 75 mg/m2 subcutaneously or intravenously, for 7 days in 28-day cycles, or placebo + AZA (PBO+AZA). Included patients were those with untreated AML, confirmed mIDH1 status and not eligible for induction chemotherapy. The primary endpoint of the study was event-free survival (EFS) defined as the time from randomisation until treatment failure, i.e. failure to achieve complete remission [CR] by week 24, relapse from remission, or death from any cause. The main secondary endpoints were the complete remission (CR) rate, overall survival (OS) and objective response rate (OOR). The researchers also examined the adverse event rates for both groups of patients.
Findings
A total of 146 patients were randomised to IVO+AZA or placebo+ AZA (PLA+ AZA) with 70 patients and a median age of 76 years randomised to IVO+AZA.
In terms of the primary outcome, EFS, this was statistically significant (hazard ratio, HR = 0.33, 95% CI 0.16 – 0.69, p = 0.0011) in favour of the IVO+AZA arm. In addition, the median OS was 24 months vs 7.9 months (IVO+AZA vs PLA+ AZA) (HR = 0.44, 95% CI 0.27 – 0.73, p = 0.0005) and CR rate with IVO+AZA was 47.2% vs 14.9% (PLA+AZA, p < 0.001), the median time to CR was 4.3 months with IVO+AZA vs 3.8 months with PLA+AZA and finally, the ORR was 62.5% vs 18.9% (IVO+AZA vs PLA+ AZA, p < 0.0001).
In terms of safety, common all-grade adverse events occurring in > 20% of patients receiving IVO+AZA vs PLA+AZA were nausea (42.3% vs 38.4%), vomiting (40.8% vs 26.0%), diarrhoea (35.2% vs 35.6%), pyrexia (33.8% vs 39.7%), anemia (31.0% vs 28.8%), febrile neutropenia (28.2% vs 34.2%), thrombocytopenia (28.2% vs 20.5%), constipation (26.8% vs 52.1%), and pneumonia (23.9% vs 31.5%).
A total of 66 (93.0%) patients receiving IVO+AZA compared with 69 (94.5%) patients receiving PLA+AZA experienced a grade ≥ 3 adverse event. Based on the recommendation of the Independent Data Monitoring Committee, further enrolment into the study was prematurely discontinued due to evidence of benefit.
The authors concluded that the IVO+AZA combination demonstrated the clinical benefit in this difficult-to-treat AML population.
Citation
Montesinos, P et al. AGILE: A Global, Randomized, Double-Blind, Phase 3 Study of Ivosidenib + Azacitidine Versus Placebo + Azacitidine in Patients with Newly Diagnosed Acute Myeloid Leukemia with an IDH1 Mutahttps://hospitalhealthcare.com/category/clinical/oncology/. ASH conference 2021