Elevated lipoprotein A levels have been found to be associated with an increased risk of total, advanced and early age onset prostate cancer
A study by researchers from the Department of Epidemiology and Biostatistics, Imperial College, London has revealed a positive association between lipoprotein A concentrations and the risk of total, advanced and early age onset prostate cancer.
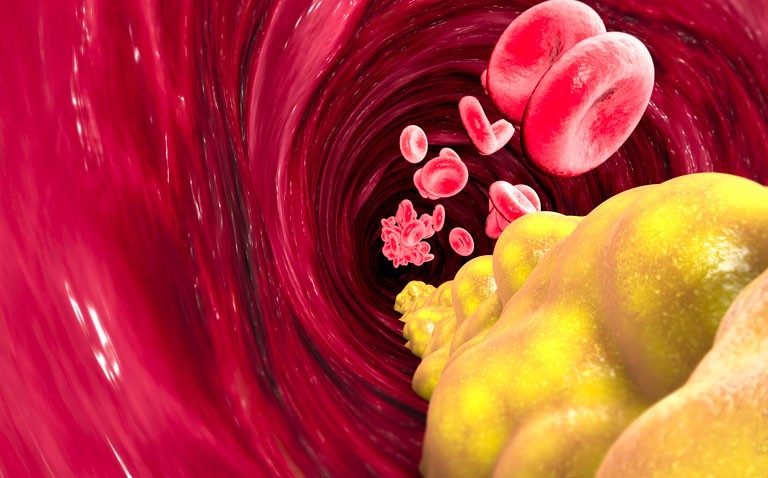
Prostate cancer is the second most common cancer diagnosis in men and the fifth leading cause of death worldwide. The GLOBOCAN 2018 data revealed how prostate cancer accounted for 7.1% of all incident cancers and 3.8% of all deaths. Moreover, there is some degree of biological heterogeneity with prostate cancer such that while there are several traditional risk factors including, age, ethnicity, family history, smoking, alcohol consumption, vasectomy and diet, the risk are different for more advanced disease. For instance, with more aggressive prostate cancer, the risk factors have mirrored those associated with cardiovascular disease such as obesity, dyslipidaemia, glucose intolerance, metabolic syndrome, unhealthy dietary habits or caloric excess, lack of physical activity and inflammation. Nevertheless, there remains much uncertainty over the precise relationship between cardiovascular risk factors and prostate cancer. For instance, though dyslipidaemia, as characterised for example, by elevated cholesterol levels, is a potential risk factor, a meta-analysis of 14 studies concluded that blood total cholesterol, HDL and LDL levels were not associated with the risk of either overall prostate cancer or high-grade prostate cancer. Furthermore, treatment for hyperlipidaemia, especially with the use of statins found that although there was no evidence that cholesterol lowering is beneficial for the prevention of low-grade or localised prostate cancer, there did appear to be an association between statin use and a reduced risk of advanced or high-grade prostate cancer. Much of the evidence for the relationship between prostate cancer and lipids comes from observational studies and one approach to control for the various confounders present in such analyses, is the use of Mendelian randomisation. In fact, one such Mendelian randomisation study assessing whether circulating lipids causally influence prostate cancer risk, concluded that there was some weak evidence to suggest that higher LDL and triglyceride levels increase aggressive prostate cancer risk.
For the present study, the UK researchers sought to determine whether genetically predicted lipid traits were associated with the overall risk of prostate cancer. They used data from the UK Biobank and looked for associations between not only cholesterol, HDL and LDL levels and prostate cancer but also with other lipid sub-fractions including lipoprotein A, apolipoprotein A and B.
Lipoprotein A and prostate cancer
Univariate analysis revealed that HLD and LDL cholesterol levels, triglycerides and apolipoprotein A and B concentrations were not associated with total prostate cancer risk. There was also no significant association between these sub-fractions and advanced prostate cancer. However, the analysis did reveal that elevated lipoprotein A levels were associated with advanced prostate cancer (odds ratio, OR = 1.03, 95% CI 1.0 – 1.06, p = 0.046) and with an increased risk of early onset prostate cancer (OR = 1.25, 95% CI 1.107 – 1.42, p < 0.001). Using multivariate analysis, the authors found that lipoprotein A levels were associated with total (OR = 1.068, p = 0.034), advanced (OR = 1.07, p = 0.055) and early onset prostate cancer (OR = 1.15, p = 0.028).
The authors concluded that their data indicated a positive association between lipoprotein A levels and the risk of total, advanced and early onset prostate cancer. In addition, they suggested that screening for high lipoprotein A levels, could be used to identify high-risk groups for prostate cancer.
Citation
Ioannidou A et al. The relationship between lipoprotein A and other lipids with prostate cancer risk: A multivariable Mendelian randomisation study PLoS Med 2022