NICE has approved crizanlizumab for the management of sickle cell crises in patients with sickle cell disease but only as part of a managed access agreement.
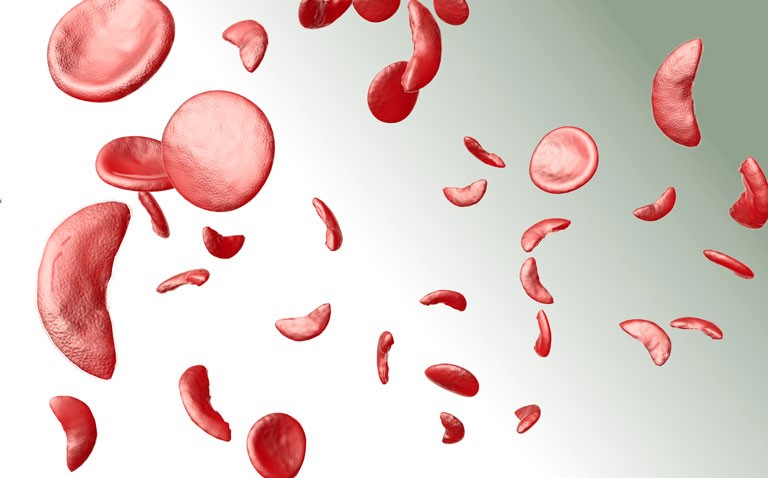
The term sickle cell disease describes a group of inherited red blood cell disorders that affect haemoglobin and which, according to the World Health Organization, approximately 5% of the world’s population carries trait genes for such disorders.
Sickle cell disease affects around 1 in 500 African American children and 1 in 36,000 Hispanic American children and is characterised by a change in the shape of red blood cells which become more ‘sickle-like”, reducing their flexibility of the cells.
These sickle-like red blood cells can lead to recurrent and unpredictable blockage of small blood vessels producing ischaemic pain, referred to as vaso-occlusion (VOC) or sickle cell crises.
In addition, activated and adherent leukocytes are the likely drivers of VOC in collecting venules and this process appears to be initiated by a transmembrane protein, P-selectin. Studies have shown that blockage of P-selectin appears to improve blood flow and thus reduce the risk of VOC and sickle cell–related pain crises.
Clinical efficacy
The monoclonal antibody crizanlizumab binds to P-selectin blocking its action. The approval by NICE was based on data from the SUSTAIN trial. This double-blind, randomised, placebo-controlled, Phase II trial, assigned 198 patients to either a low-dose crizanlizumab (2.5 mg per kilogram of body weight), a high-dose crizanlizumab (5.0 mg per kilogram), or placebo and which were administered intravenously 14 times over a period of 52 weeks.
The primary outcome was the annual rate of sickle cell–related pain crises with high-dose crizanlizumab versus placebo. For the study, this was defined as acute episodes of pain caused by a VOC that resulted in a visit to a medical facility and treatment with pain relief medication.
The results showed that the median rate of crises per year was 1.63 with high-dose crizanlizumab versus 2.98 with placebo (p = 0.01). In addition, the median time to the first crisis was significantly longer with high-dose crizanlizumab than with placebo (4.07 vs. 1.38 months, p = 0.001),as was the median time to the second crisis (10.32 vs. 5.09 months, p=0.02).
In addition, the overall incidence of serious adverse event was comparable across the three arms.
NICE recognised that a limitation of the trial was the absence of longer term data on crizanlizumab such as mortality or among those who did not seek medical advice on VOCs. There was also no data on the prolonged treatment benefit and what happens when patients stop taking crizanlizumab.
While the appraisal document concluded that “Crizanlizumab is not recommended for routine use in the NHS“, the drug could be used where specific criteria are met. Thus, guidance notes that “crizanlizumab is recommended as an option for preventing recurrent sickle cell crises (vaso-occlusive crises) in people aged 16 or over with sickle cell disease only if the conditions in the managed access agreement are followed.”
Source. NICE 2021