The identification of clinical markers for vaccine-induced immune thrombocytopenia and thrombosis may help to guide effective management.
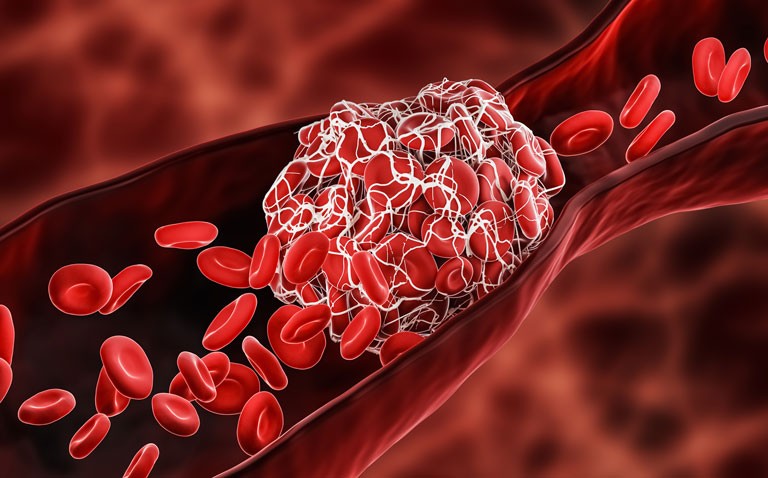
One of the most commonly used COVID-19 vaccines is ChAdOx1 made by AstraZeneca and since rollout of the vaccine in the UK in January 2021, millions of doses have been administered around the world. The ChAdOx1 vaccine has been found to be safe and able to induce a satisfactory antibody response. Though it is generally accepted that no vaccine is completely free of adverse effects, concerns over vaccine-induced thrombocytopenia (VITT) associated with ChAdOx1 appeared in June 2021. In one of these reports, doctors identified five cases of venous thrombosis and thrombocytopenia, 7–10 days after patients had received their first dose of the vaccine and proposed that this was a rare vaccine-related immune response. Nevertheless, this was not an isolated finding and a second report identified clinical and laboratory findings in 11 patients who had developed either thrombosis or thrombocytopenia, again 5–16 days after receipt of their first vaccine. Moreover, a common feature of both these reports was how in all cases, patients were previously fit and heathy. This adverse effect has been termed vaccine-induced thrombocytopenia and thrombosis (VITT) and shares clinical features with heparin-induced thrombocytopenia.
Due to the appearance of these cases, a group from the Department of Haematology, Oxford University Hospitals, UK, convened an expert haematology panel to evaluate patients, discuss treatment and develop consensus management guidelines. Data capture was made using an anonymised electronic reporting form submitted by a total of 182 consultant haematologist presented cases from 96 NHS trusts across the UK. The form included information on the presenting features, initial treatments, thrombosis site, any laboratory measures and associated patient outcomes. A case of VITT was defined as one where symptoms occurred within 5 to 30 days after vaccination, the presence of thrombosis, thrombocytopenia, a D-dimer level above 4000 and the presence of antibodies to platelet factor 4.
Findings
A total of 294 patients were included, of which there were 170 definite and 50 probable cases of VITT, occurring a median of 14 days after the first dose of the ChAdOx1 vaccine. The median age of patients was 48 years (55% female) and the majority (91%) of white ethnicity. Previous medical histories were available for 165 patients, of whom, 41%, had no prior medical problems and no patients had been exposed to heparin in the three months prior to their onset of VITT. The most common thrombotic site was the cerebral veins (50%). Overall mortality was 22% and the odds of death was increased 2.7-times among those cerebral thrombosis (odds ratio, OR = 2.7, 95% CI 1.4–5.2). In addition, mortality was also increased (OR = 1.7) for every 50% decrease in baseline platelet count and also by 1.7 for every increase of 10,000 in the baseline D-dimer level.
Commenting on these findings, the authors noted how the results had shown that baseline platelet count and the presence of an intracranial haemorrhage were independently associated with death. They concluded that the identification of these two potentially prognostic markers could help guide effective management of the condition.
Citation
Pavord S et el. Clinical Features of Vaccine-Induced Immune Thrombocytopenia and Thrombosis. N Engl J Med 2021