An exercise stress test that had fallen out of favour due to its perceived inaccuracies has shown precision in identifying abnormalities in the vessels supplying the heart muscle with blood in a new study.
The electrocardiogram exercise stress test (EST) was historically validated against the demonstration of obstructive coronary artery disease (oCAD) but has been downgraded in international guidelines due to a high false positive rate.
However, researchers from King’s College London (KCL) pointed out that myocardial ischemia can occur because of coronary microvascular dysfunction (CMD) in the absence of oCAD.
Published in the Journal of the American College of Cardiology, the study therefore assessed the specificity of EST to detect an ischemic substrate against the reference standard of coronary endothelium-independent and endothelium-dependent microvascular function in patients with angina with nonobstructive coronary arteries (ANOCA).
The researchers found ischemia on EST was highly specific of an underlying ischemic substrate in patients with ANOCA.
‘Far-reaching implications’ for diagnosis with EST
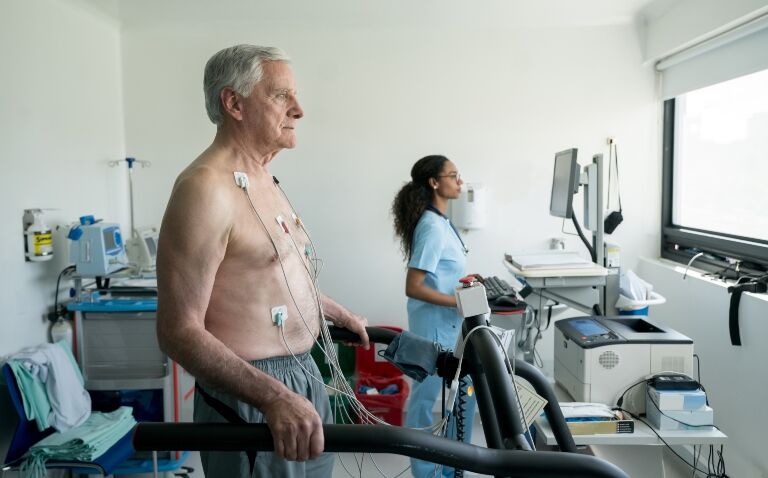
Some 102 patients (65% women, mean age 60 ± 8 years) with ANOCA underwent a comprehensive assessment of the function of both the large and small blood vessels before going on to carry out an EST.
A total of 32 patients developed ischemia (ischemic group) during EST and 70 patients did not (nonischemic group); both groups were phenotypically similar.
Ischemia during EST was 100% specific for CMD. Acetylcholine flow reserve was the strongest predictor of ischemia during exercise.
Using endothelium-independent and endothelium-dependent microvascular dysfunction as the reference standard, the false positive rate of EST dropped to 0%.
All patients in the ischemic group would have been classified as having an inaccurate test in the past, as all of these patients had normal large blood vessels.
However, each patient who had evidence of blood supply/demand mismatch on their EST had abnormalities in their small blood vessels.
The researchers concluded that an abnormal EST is accurate in identifying patients who have abnormalities in their large and/or small blood vessels supplying the heart muscle.
‘These findings challenge the traditional belief that EST has a high false positive rate,’ they said.
Dr Aish Sinha, first author of the study and PhD student at KCL, said: ‘This study has far-reaching implications as it may make a currently difficult to diagnose condition far easier to identify and, subsequently, treat. These hypotheses warrant further randomised trials to answer them.’
He added that the findings may also influence ‘the way in which we view the diagnostic accuracy of all non-invasive tests’.
And he questioned whether all non-invasive modalities should, in fact, ‘now be validated against the contemporary reference standard of comprehensive coronary physiology assessment’.