Coronary artery calcium scores and cystatin C levels offer prognostic value for risk stratification and adverse cardiac event prediction
Combining a patient’s coronary artery calcium score and their cystatin C level provides an incremental risk assessment of major adverse cardiac and cerebrovascular events (MACCEs) and all-cause death, in patients symptomatic with chest pain according to the findings of a study by Chinese researchers.
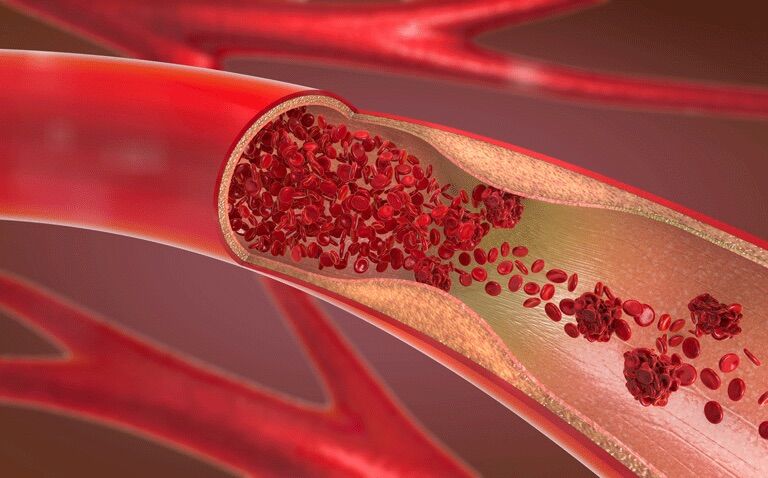
The World Health Organisation describes how cardiovascular diseases are the leading cause of global deaths, with an estimated 17.9 million lives lost each year. Consequently, risk stratification tools are required to inform on the subsequent management decisions for patients. One such measure to assist in cardiovascular disease risk stratification is the coronary artery calcium (CAC) score, which is a highly specific feature of coronary atherosclerosis. In fact, the extent of CAC has been shown to accurately predicts 15-year mortality in a large cohort of asymptomatic patients. Another potentially useful marker is Cystatin C (Cys-C) which is cysteine protease inhibitor produced at a constant rate by all nucleated cells and used as a sensitive marker of renal function. Moreover, Cys-C has been found to be a strong predictor of the risk of death and cardiovascular events in elderly patients.
Given the potential and independent value of these markers for predicting the risk of a cardiovascular event, the Chinese researchers wondered if there was an association between baseline CAC scores and Cys-C levels and both MACCEs and all-cause death in symptomatic, chest pain patients. They included all individuals presenting with symptomatic chest pain suggestive of CHD and who were referred for cardiac computed tomography (CT) by their cardiologists, which enabled assessment of the coronary artery calcium score. Based on the CT findings, patients were classified into two groups: those with CAC scores < 100 or CAC scores ≥ 100. Blood samples were taken to measure Cys-C levels and risk stratification of CAC score and Cys-C level were as follows: low risk (CAC score < 100 or Cys-C < 0.995 mg/L. and high risk (CAC score ≥ 100 or Cys-C ≥ 0.995 mg/L).
Coronary artery calcium and cysteine C levels and MACCEs
A total of 7140 participants with a median age of 63 years (64.9% male) were included and followed for a median of 1,106 days. During the period of follow-up, 305 MACCEs and 191 all-cause death events were observed.
A higher incidence of MACCEs were independently associated with CAC scores ≥ 100 (hazard ratio, HR = 1.46, 95% CI 1.15 – 1.85, p = 0.002) and where Cys-C levels were ≥ 0.995 mg/L (HR = 1.57, 95% CI 1.24 – 2.00, p < 0.001).
When categorised as high risk (i.e., CAC score ≥ 100 or Cys-C ≥ 0.995 mg/L), patients also had a significantly increased risk of MACCEs (HR = 2.33, 95% CI 1.64 – 3.29, p < 0.001). In addition, this high risk pattern was also associated with a significantly greater risk of all-cause mortality (HR = 2.85, 95% CI 1.79 – 4.55, p < 0.001). In fact, even in patients with CAC scores of < 100 but a Cys-C ≥ 0.995 mg/L, there was an increased risk of MACCEs (HR = 1.76, p = 0.003) and all-cause mortality (HR = 2.02, p = .007).
The authors concluded that the combined stratification of CAC score and Cys-C showed an incremental risk of MACCEs and all-cause death thus reflecting complementary prognostic value of these measures.
Citation
Luo F et al. Coronary artery calcium and cystatin C for risk stratification of MACCEs and all-cause death in symptomatic patients. Clin Cardiol 2022