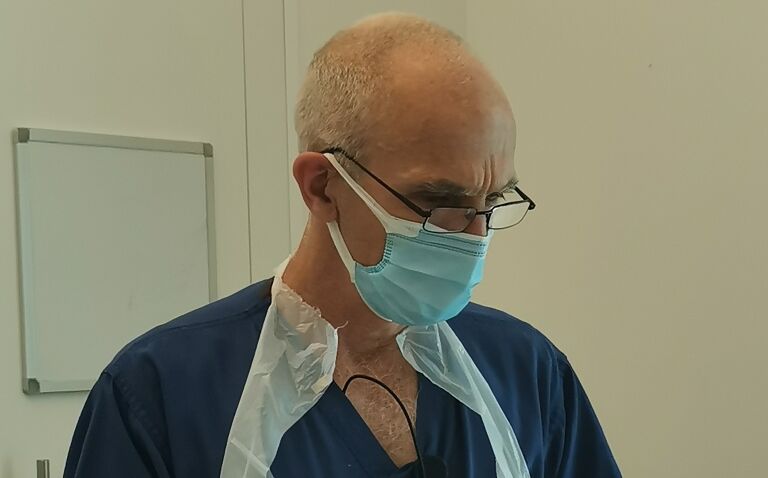
Stephen Taylor PhD is a critical care and research dietitian based in the ICU department at Southmead Hospital, North Bristol NHS Trust. He has spent many years exploring the use of enteral feeding and more recently on optimising the insertion of feeding tubes, which he stresses should be deemed a specialist rather than routine procedure based on the associated high level of risk.
With around 6% of hospital patients requiring invasive nutritional support, particularly with nasogastric feeding, tube insertion has become a relatively common intervention.
This, according to Stephen Taylor PhD, critical care and research dietitian at Southmead Hospital, North Bristol NHS Trust, means that the procedure is deemed to be of low risk, which is simply not the case. ‘Most people don’t realise that placing a nasogastric tube, the easiest to do, has about the same morbidity and mortality as a tracheotomy,’ he says.
Dr Taylor believes that in an ideal world, there should be small teams and who are ‘expertly trained in guided tube placements, either electromagnetic, direct vision or both.’
Interestingly, he cites published data showing that centres with a low use of electromagnetic tube placement have ‘a worse rate of undetected misplacement than blind placement’. However, the overall use of guided-tube placement results in a lower incidence of pneumothorax than blind placement. This is because in most cases misplacement is detected during placement, when most complications occur.
Regulatory barriers
Unfortunately, regulatory bodies only permit pH and X-ray as the end-of-procedure checks. Despite the success of guided-tube placement, these methods are really only perceived as acceptable ‘add-ons’ that increase the overall procedural costs. But, as Dr Taylor explains, this serves only to discourage clinicians from using them even though these are the only techniques that ‘prevent those lung complications and oesophageal misplacements that would otherwise happen and would only be detected at the very end.’
Evidence from studies where these more sophisticated techniques have been used by untrained hands, ‘has led to major complications’, says Dr Taylor. As a result, rather than mandating high quality training, regulatory authorities have simply suggested that these techniques cannot be relied upon.
Correct tube insertion
So, how does a clinician know if they have inserted a tube correctly? Dr Taylor first highlights the importance of tube tracking. After all, once it ‘hits the greater curvature of the stomach it could then coil back towards the oesophagus’, he says. Hence, without some means of tracking, it is impossible to know the precise location of a tube.
While it seems intuitive and rather obvious that some form of tube tracking is required, Dr Taylor describes how ‘more than 95% of tubes in most centres are placed blindly’ – that is to say, unguided. Once a tube is placed beyond the mouth or nose, ‘you no longer know where the tube is’, Dr Taylor explains. He adds that although sophisticated tracking devices are available, ‘such devices are used in less than 5% of all the tubes that are placed’.
Although a patient’s response, such as coughing, quickly alerts a clinician that a tube may be traveling down the respiratory tract, there remains uncertainty over the precise location of the tube. In the absence of a tracking system, several end-of-procedure checks are used to help identify tube misplacements, for instance, if a tube has inadvertently entered the thorax, by which time a pneumothorax may have occurred or, at the least, the tube must be re-positioned and re-confirmed,’ Dr Taylor says.
End-of-procedure checks
One check, for example, relies on determining the pH of the surrounding fluid. A small amount of fluid is aspirated and the pH checked with the acceptable range – set s anywhere between a pH of 4.0 and 5.5. At his own centre, Dr Taylor and his team use a pH of 4.0 simply because this indicates that the tube is more likely to be within the stomach and not the distal oesophagus where, in practice, the pH might be above 4.0.
An alternative end of procedure check is the use of X-rays, which are deemed the gold standard. Sometimes, clinicians will also use a mid-procedure X-ray check, which allows the operator to identify whether the tube has become lodged in the respiratory tract rather than the alimentary canal.
Although this mid-procedure x-ray has some value, Dr Taylor thinks that a downside to these additional checks, which require movement of the patient to the X-ray room and a slightly higher exposure to radiation, is that it will delay the medication and feeding by hours, sometimes a day.
Another increasingly used mid-procedure check relies on the measurement of carbon dioxide. After insertion of the tube by only 30-35cm, the tube is aspirated to check for CO2 with either colorimetric paper or a meter. If the CO2 reading is high, this is a clear indication that the tube is within the respiratory tract, allowing the operator to withdraw the tube.
Electromagnetic tracking can also be used. This more sophisticated technique allows the operator to visualise the path followed by the tube on a computer screen. Additionally, several direct visual methods are also available.
Currently, pH and chest X-ray checks are the standard practice to prevent undetected misplacements, Dr Taylor confirms.
Risk of damage from blind tube placement
End-of-procedure checks designed to ensure that a feeding tube has reached its intended location are the only checks mandated and endorsed by regulatory authorities.
Nevertheless, Dr Taylor feels that the focus on detection of tube misplacements ignores a more important problem: the damage that might occur during blind tube placement. ‘Undetected misplacements occurs in only 0.015% of tube placements,’ says Dr Taylor. While these can result in a pneumothorax, pneumonia and even death, they represent a small proportion of tube-related respiratory complications. The current end-of-procedure checks fail to recognise any direct damage from respiratory placement.
Bu comparison, ‘some 1.6% of tubes enter the respiratory tract resulting in 0.49% causing a pneumothorax,’ Dr Taylor says, ‘so 97% of tube-related major complications and/or death. These cannot be prevented by using an end-of-procedure – pH or X-ray – checks because they have already occurred before checking.’ In other words, end-of-procedure checks only ensure that food, water or medications are delivered to the correct location. Such checks cannot identify any trauma caused by insertion of the tube.
Dr Taylor airs concern that in reality most of the risks to patients arise from tube insertion and ‘none of the major bodies have addressed this in their guidelines’.
Room for improvement
There is still a need to reduce the level of misplacements, but Dr Taylor believes this will only occur if regulatory bodies accept that risks arise not only from undetected misplacement but also from trauma during respiratory tract misplacement and oesophageal misplacement that pH can fail to detect.
Regulatory authorities need to sanction the use of guided placement by an expert, says Dr Taylor. But this, he adds, would require the regulator to ‘nationally mandate evidence-based guidance and training to attain expertise in guided methods’.
He is hopeful that in future the mid-procedure CO2 screening will become standard, and that guided tube placement will become more common. Drawing a parallel with the insertion of coronary artery stents, which is a guided procedure, he thinks it nonsensical for feeding tubes to be routinely inserted without any such guidance. His hope is for the development of a system that enables direct vision of the tube combined with a tracking system showing the tube’s path.
Though electromagnetic tracking and direct vision have been available for many years, it remains expensive. Dr Taylor thinks that the technology is under-used because the focus of guidelines is on reducing undetected misplacements and not on complications. Nevertheless, while guided techniques are expensive, the costs associated with complications such as a pneumothorax are even higher, and this must be considered.
Finally, Dr Taylor reflects on how for too long the insertion of feeding tubes has become seen as a routine rather than specialist procedure. Consequently, clinical staff remain largely ignorant of the potential risks and complications associated with the procedure and there is an urgent need to change this mindset.