A systematic review and meta‐analysis found that tafasitamab showed the best efficacy in relapsed/refractory diffuse large B-cell lymphoma
According the findings of a systematic review and meta-analysis undertaken by Korean researchers and presented at the American Society of Haematology conference, 2022, tafasitamab showed a trend for best efficacy among failed autologous stem cell transplantation (ASCT) or ineligible relapsed/refractory diffuse large B-cell lymphoma (DLBCL) patients.
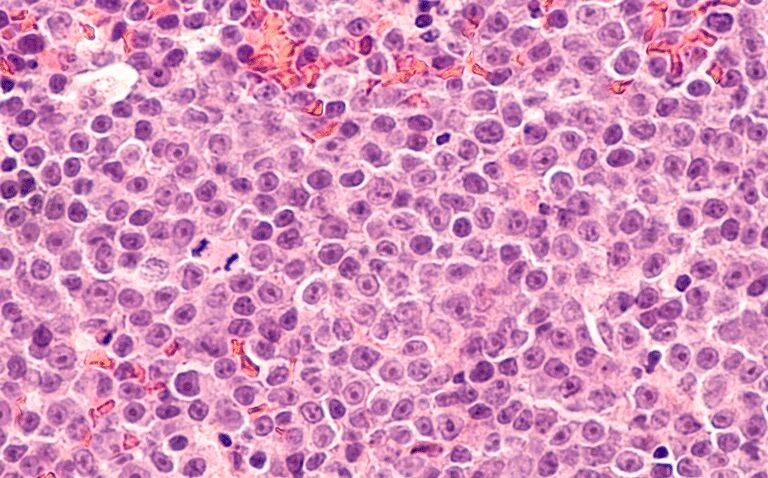
Diffuse large B cell lymphoma is the most common lymphoma, accounting for about 25% to 30% of all the non-Hodgkin lymphomas and which presents as a rapidly growing mass or enlarging lymph nodes in a nodal or extra-nodal site. Non-Hodgkin lymphomas account for about 80% of all lymphomas and while there are more than 30 subtypes, the common ones are diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma. Although 5-year survival rates range from 60% to 70%, up to 50% of patients become refractory to or relapse after treatment. Moreover, outcomes for refractory or relapsed patients are poor, with one study of 861 patients, 636 of whom had refractory disease, finding that the median overall survival was 6.3 months and that only 20% of patients were alive at 2 years. For patients with relapsed/refractory disease, there are several combination chemotherapy regimens available including tafasitamab-cxix, polatuzumab vedotin-piiq, bendamustine as well as CAR T cell therapies. Nevertheless, the most effective treatment remains to be determined.
In the present study, the Korean researchers performed a systematic review and meta‐analysis to identify prospective phase II or III clinical studies evaluating the efficacy of treatments for ASCT-failed or ineligible relapse/refractory DLBCL patients. They used random effects models to estimate one-year progression-free survival rate, complete remission rate, and subgroup differences. In addition, meta-regression models were performed with adjustment for relevant covariates, particularly the median number of previous lines of systemic therapy and CAR T cell therapy was used as a reference treatment in the meta-regression analysis.
Tafasitamab and one-year progression-free survival
The researchers identified 56 cohorts in 50 studies with 3,544 relapsed/refractory DLBCL patients. For the analysis, treatment regimens were divided into nine groups: CAR T cell therapy, chemotherapy, lenalidomide-based therapy, ibrutinib-based therapy, tafasitamab-based therapy, polatuzumab plus bendamustine and rituximab (pola-BR), loncastuximab, selinexor, and others.
The pooled one-year progression-free survival rate was 0.40 (95% CI 0.35 – 0.46) for CAR T cell therapy, 0.23 (95% CI 0.16 – 0.30) for chemotherapy, 0.28 (95% CI 0.19 – 0.37) for lenalidomide and 0.46 (95% CI 0.37 – 0.56) for tafasitamab.
Although CAR T cell treatment was significantly better than many of the others, in fact, loncastuximab, pola-BR, and tafasitamab were all shown to have no significant difference in efficacy to CAR T cell therapy after adjustment for the median number of prior lines of treatment in the meta-regression analysis.
The authors concluded that tafasitamab showed a trend of best efficacy and that CAR T cell therapy was no more effective than tafasitamab, loncastuximab or pola-BR. However, because of the high level of heterogeneity, the authors called for randomised controlled trials to confirm their findings.
Citation
Kim J et al. Comparison of Several Salvage Treatments of Relapsed/Refractory Large B-Cell Lymphoma Including Chimeric Antigen Receptor T-Cell Therapy: A Systematic Review and Meta‐Analysis. Abstract 2986 ASH conference 2022