Ultrasonography guided femoral access for coronary angiography did not lower bleeding or vascular problems compared to fluoroscopy alone
Using ultrasonography guided femoral access in coronary angiography interventions does not result in a lower rate of major bleeding or vascular complications compared to the use of fluoroscopy alone according to the findings of a randomised, controlled trial by Canadian researchers.
The results of a meta-analysis of 31 trials suggested that the use of radial access for coronary angiography and percutaneous coronary interventions is associated with a significant risk reduction in bleeding, vascular complications, and mortality compared to femoral access, though the risk of stroke or myocardial infarction are comparable.
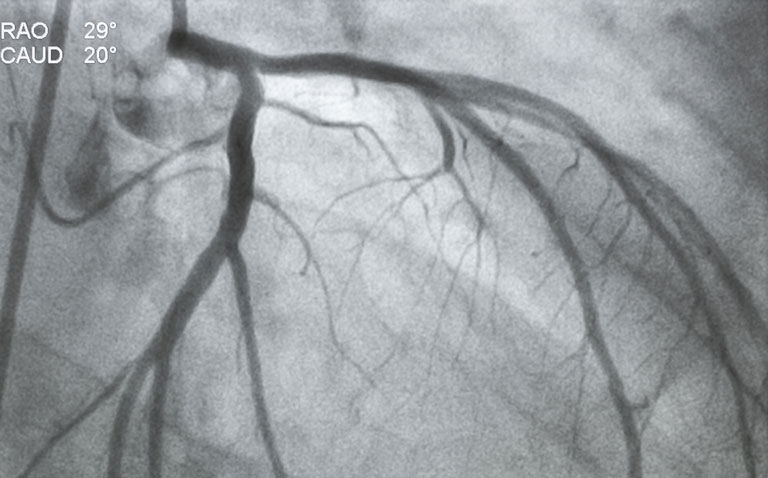
Nevertheless, the femoral artery is commonly used for diagnostic angiography and for percutaneous coronary interventions and especially if the radial arteries are either too small or occluded. Ultrasonography (US) enables direct visualisation of the critical landmarks for access such as the inguinal ligament, the femoral head and this allows the operator to select the optimal location for vascular access.
However, the evidence that US is beneficial is mixed. For example, in one randomised controlled trial, routine real-time US guidance improved common femoral access (CFA) cannulation only in patients with high CFA bifurcations whereas in another, ultrasound guidance did not reduce the primary outcome which was a composite including major bleeding and major adverse cardiovascular events compared to the standard technique.
Moreover, evidence from a survey of 68 interventional cardiologists found that only 13.3% reported using ultrasound routinely despite widespread availability and technical expertise.
For the present study, the Canadian team undertook a randomised trial to compare guidance for femoral artery access using fluoroscopy either with or without ultrasonography. Eligible patients were those undergoing coronary angiography or a percutaneous coronary intervention and with planned femoral access and randomised 1:1 to either intervention.
The non-US group used only palpation and fluoroscopy to identify the femoral ahead prior to puncturing the artery. The primary outcome was the composite of Bleeding Academic Research Consortium (BARC) 2, 3 and 5 bleeding or major vascular complications (including femoral artery pseudo-aneurysm and arteriovenous fistula) within 30 days.
Ultrasonography and femoral access bleeding
A total of 621 patients with a mean age of 71 years (25.4% female) were randomised to either ultrasonography and fluoroscopy (311) or fluoroscopy alone.
The primary outcome occurred in 12.9% of patients using US and 16.1% using fluoroscopy alone and this difference was not significant (odds ratio, OR = 0.77, 95% CI 0.49 – 1.20, p = 0.25). Similarly, the BARC 2, 3 and 5 bleeding were also not significantly different (OR = 0.93, 95% CI 0.55 – 1.56, p = 0.78).
As with bleeding, the rates of vascular complications were also not significantly different between the two groups (6.4% vs 9.4%, OR = 0.67, 95% CI 0.37 – 1.20, p = 0.18).
However, the use of US did significantly improve the first-pass success (OR = 2.76, 95% CI 1.85 – 4.12, p < 0.01) and reduced the number of arterial puncture attempts (mean difference = -0.26, p < 0.01) although access times were not different.
The authors concluded that while ultrasonography guided femoral access did not reduce bleeding or vascular complication rates compared to fluoroscopy, there was a significant difference in the risk of venipuncture and the number of attempts. The authors called for further studies to demonstrate additional potential benefits of US-guided access.
Citation
Jolly SS et al. Routine Ultrasonography Guidance for Femoral Vascular Access for Cardiac Procedures: The UNIVERSAL Randomized Clinical Trial JAMA Cardiol 2022