Taking a probiotic yogurt drink alongside antibiotics has been found to attenuate the antibiotic-induced gut microbiota disturbance.
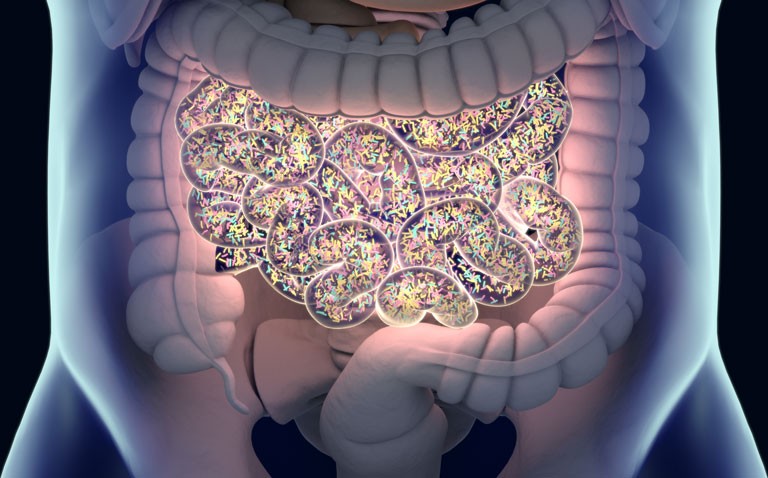
The gut microbiota refers to the community of bacterial species within the intestines and plays an important role in the overall health of the host. With approximately 100 trillion micro-organisms, the gut microbiota can be thought of as a virtual organ of the body that impacts on immune, metabolic and neurobehavioral traits. This wide range of effects on the host’s health are thought to be mediated by short-chain fatty acids (SCFAs), the main metabolic products of gut micro-organisms from the fermentation of dietary fibres and resistant starches.
Alterations in the gut flora are thought to be the main reason for diarrhoea, which is a common side-effect of antibiotics. One way of minimising antibiotic-induced diarrhoea is through the use of probiotics and in a 2017 systemic review, the pooled incidence diarrhoea was reduced to 8% in those using probiotics compared to 17.7% in the control group. However, what is less clear, is the impact of a probiotic on faecal levels of SCFAs and whether the use of probiotics alongside antibiotics can mitigate the changes in gut microbiota following a course of antibiotic treatment.
This was the question posed by a team from the Department of Family Medicine, Georgetown University Medical Centre, Washington, US. They set out to determine whether a yogurt containing the probiotic, Bifidobacterium animalis subsp. Lactis BB-12 (BB-12), could protect against the antibiotic-induced disruptions in both faecal SCFAs levels and gut microbiota composition. The undertook a randomised, controlled trial, in all participants received a 7-day course of amoxicillin-clavulanate 875 mg twice daily. The intervention group received a 14-day supply of a probiotic yogurt with BB-12 and the other group a control yogurt although participants were blinded to which yogurt they received. Faecal samples were collected and analysed for SCFAs and gut microbiota composition at baseline and then after 7, 14, 21 and 30 days. The primary measure of interest was changes in the level of the SCFA, acetate.
Findings
A total of 56 individuals with a mean age of 29.4 years (gender was not reported) were randomised in a 2:1 fashion to either BB-12 yogurt (38) or control. There was a significant decrease in the primary measure following administration of the antibiotics of 20.3% on day 7 in the control group. In contrast, in the BB-12 group, the corresponding reduction was lower at 15.6%. However, by day 30, acetate levels in the control group were still 25.1% lower than baseline values but only 1.6% lower in the BB-12 group. Using a measure of gut microbiota diversity, the authors found that at days 21 and 30, there was a greater decrease in diversity in the control compared to the BB-12 group.
From the participant perspective, by day 7, 42% of the control group reported at least one day of loose stools compared to 26% in the BB-12 group.
The authors concluded that concurrent administration of BB-12 with antibiotics was associated with a significantly smaller decrease in faecal SCFA levels and a more stable gut microbiota over time compared to a control yogurt.
Citation
Merenstein D et al. Bifidobacterium animalis subsp. lactis BB-12 Protects against Antibiotic-Induced Functional and Compositional Changes in Human Fecal Microbiome. Nutrients 2021