An international consensus panel led by researchers from The Westmead Institute for Medical Research has highlighted the need to redefine non-alcoholic fatty liver disease (NAFLD).
This will be renamed metabolic associated fatty liver disease (MAFLD) and researchers highlighted that the new terminology will better reflect its causes, and improve public health initiatives.
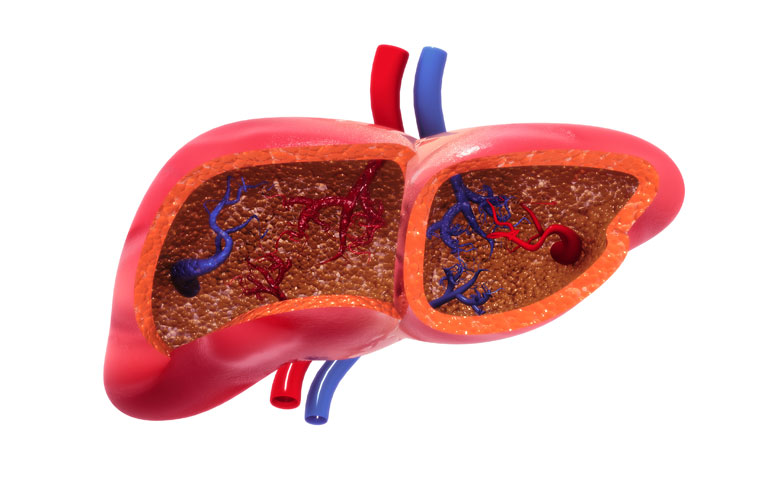
MAFLD is a condition characterised by a build-up of fat in the liver and affects over one billion people. Over time, this can lead to complications including cirrhosis, liver failure, liver cancer, and heart health issues.
The consensus panel found that both the term ‘NAFLD’ and its diagnostic criteria must be updated in order to better reflect our current understanding of the disease.
Associate Professor Mohammed Eslam, co-lead author of the paper said, “Since it was first described in 1980, we haven’t revisited the appropriateness of the name, or the criteria used to diagnose fatty liver disease.
“By updating terminology and definitions, we can shift towards more precise and personalised treatment pathways, trial design and drug development.”
Professor Jacob George, co-lead author of the paper said, “Initially, the disease was defined as fatty liver in the absence of significant alcohol intake. This definition was problematic and has resulted in a ‘one-size-fits-all’ approach to treatment, despite the significant variation we see in people affected by the disease.
“This may be one of the reasons why we are seeing relatively low response rates in our current trials.
“The proposed name and definition recognises that the disease we are looking at is associated with metabolic dysfunction. It also acknowledges that there are multiple overlapping causes and drivers of the disease.”
Researchers are now conducting further studies to characterise the different sub-types and causes of MAFLD to help design new clinical trials, and best practices for patient management.
“Ultimately, we hope that by strengthening the diagnostic criteria and language surrounding MAFLD, we can help reduce the progression of the disease, and reduce the number of people affected worldwide,” Professor George concluded.