A new guideline on the treatment of drug-resistant tuberculosis (DR-TB) has been published.
The guideline from The American Thoracic Society, Centers for Disease Control and Prevention, European Respiratory Society and the Infectious Diseases Society of America makes new recommendations for the choice and number of drugs, as well as the duration of treatment for DR-TB. These recommendations prioritise the use of medications that can be administered orally.
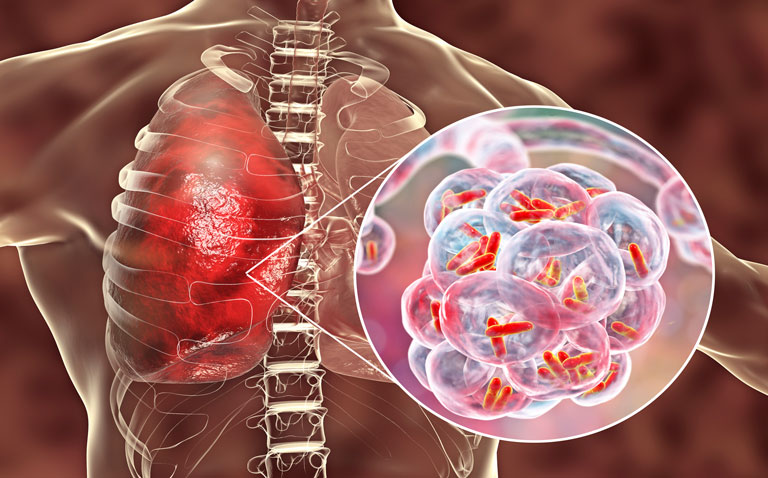
The guideline makes clear that treatment should be tailored based on drug-susceptibility testing, and that individuals should not receive medicines to which the Mycobacterium tuberculosis strain is resistant.
The guideline includes two other new recommendations. It recommends treatment with a later-generation fluoroquinolone of all infected contacts of multidrug-resistant tuberculosis (MDR-TB) patients, rather than watchful observation, and it provides evidence-based guidance for the treatment of pregnant women with MDR-TB for the first time.
Treatment for MDR- and extensively drug-resistant (XDR)-TB is long and difficult. The availability of potent new and repurposed medicines allows practitioners, for the first time, to choose alternatives to injectable drugs, which have long been considered an essential component of treatment regimens for DR-TB. These injectable drugs have well-known toxicities, including irreversible hearing loss.
By prioritising the use of orally administered medicines, the guideline writing committee believes clinicians can spare patients some of the most debilitating effects of TB treatment, make treatment more tolerable and improve outcomes.
The guideline committee included specialists in pulmonary medicine, infectious diseases, paediatrics, primary care, public health, epidemiology, economics, pharmacokinetics, microbiology, systematic review methodology and advocacy.
“Having the participation of committee members from multiple medical societies and the CDC, as well as patient advocate perspectives, was absolutely critical to discussing the balance between desirable and undesirable health effects of interventions, making certain they were favourable for MDR-TB patients, including for children and pregnant women,” said Payam Nahid, MD, MPH, chair of the guideline committee and a professor of medicine at the University of California, San Francisco.
This guideline is generally consistent with the World Health Organization’s recommendations but includes some different recommendations that are specifically tailored to low-incidence, higher-resource countries of North America and Europe.
In making its recommendations, the committee reviewed findings from 50 studies, conducted in 25 countries involving more than 12,000 patients with DR-TB.
The committee grouped questions to be answered by the guideline into six topics:
1) number of effective drugs in a regimen for DR-TB, duration of intensive and continuation phases of treatment for DR-TB;
2) review of drug and drug classes for the treatment of DR-TB;
3) the use of a standardised, shorter-course regimen of < 12 months for the treatment of MDR-TB;
4) treatment of isoniazid-resistant, rifampin-susceptible TB;
5) surgery as adjunctive therapy for MDR-TB; and
6) treatment of contacts of persons with MDR-TB.
The committee used the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) framework to indicate the strength of the evidence supporting the 25 recommendations included in the clinical guidance.
“The individual patient data level analyses conducted by investigators at McGill University were essential to the development of our recommendations, representing a substantial analytic advance over prior approaches that relied on aggregate data,” said Barbara Seaworth, MD, guideline committee co-chair and medical director of the Heartland National TB Center, at the University of Texas Health Science Center at Tyler. “However, the certainty in the evidence for observational studies is lower than for clinical trials, and much greater investment is urgently needed to allow the TB research community to conduct high-quality randomised, interventional TB clinical trials that will define safe and effective all-oral regimens for treatment of all patients with DR-TB.”