Many hospitals with active oncology departments require access to pathology laboratories to enable a complete molecular profile of a tumour from relevant biopsies. At the same time, new drugs for targeted therapy and immunotherapy are becoming available and many of them are used in combination or sequentially to avoid resistance mechanisms. However, a consequence of this revolution in cancer treatment is that a new challenge is looming on the horizon for the pathologists: that is, to work beyond the diagnosis and classification and directly contribute to optimising rapid patient treatment with sustainable costs.
The choice of analytical methods depends on clinical requirements, availability of space, expertise of the staff and dedicated budget. In our Unit, we chose a multimarker-approach based on next generation sequencing (NGS) platforms (for example, ThermoFisher Scientific). Serial testing takes time and depletes tumour tissue and the cost of single-gene methods scales linearly with the number of interrogated genes, which led us to choose our current approach. The ASCO endorsement of the College of American Pathologists/International Association for the Study of Lung Cancer/Association for Molecular Pathology Clinical Practice Guideline Update1 stated that multiplexed panels are likely to be more efficient in terms of cost and tissue requirements than other technologies.
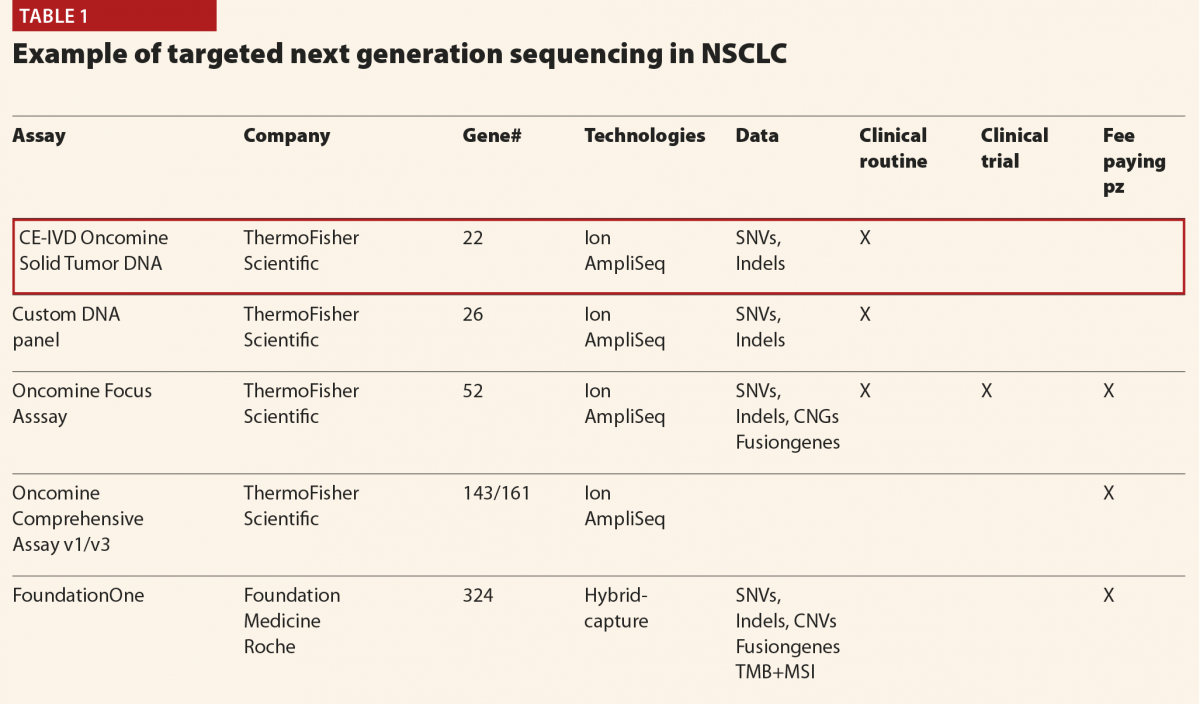
Currently we receive 4000 requests of molecular tests per year mainly for advanced solid tumours (non-small cell lung cancer (NSCLC), colorectal carcinomas and malignant melanomas represent 80% of the samples). A panel of 22 genes (Oncomine Dx Solid Tumors) is offered to all the patients, whereas more complex panels (Oncomine Focus and Oncomine Comprehensive Assays) identifying not only mutations but also copy number variations, and fusion genes can be used in selected cases
(Table 1).
Immunotherapy is transforming oncology and its use in many solid tumours and Hodgkin’s lymphoma has become a stronghold in the changing landscape of cancer treatment. Immune checkpoint inhibition is exemplified by the introduction of anti-PD-1 or anti-PD-L1 antibodies. The evaluation of PD-L1 expression in tumour cell sand/or inflammatory cells is the most widely used predictive assay. However PD-L1 has a heterogeneous expression pattern and different antibodies are available for this assessment. There are different evaluation schemes in different tumours to assess PD-L1 positivity and match the patient to the therapy. Moreover, it is well known that some patients having tumours with high PD-L1 expression might show hyper-progression during anti-PD1–PD-L1 therapy. To overcome these issues, a potential biomarker has been introduced recently: namely, the tumour mutation burden (TMB).
Patient-specific neoantigens that develop as a result of somatic mutations can induce a T-cell response. A high number of mutations does not always result in neoantigens, but it does increase the probability of developing neoantigens. This observation is promising as studies have shown that mutational landscape determines sensitivity to PD-1 blockade in NSCLC and that PD1 inhibitors in patients with a higher non-synonymous TMB in their tumours have a greater efficacy. We now know that it is possible to use wide NGS panels instead of whole exome sequencing to calculate TMB, but there are great differences in NGS gene panel content, variant filtering methods and definitions of high TMB thresholds. So it is difficult to compare TMB results across studies. In clinical practice, we need an ‘all in one assay’ to give a complete answer to the patient and to the oncologist. For a complete evaluation of the genetic aberrations present in the tumour sample (mutations, copy number alterations, fusion genes, TMB and MSI) there are only two validated and FDA approved NGS panels: Foundation One Dx and MSKCC Impact. However, the epidemiology of NSCLC makes it impossible to use these assays in all the cases. Other panels are currently available (ThermoFisher, for example) or soon to be available (Illumina panel with 500 genes). In Europe, we are not obliged to work with companion diagnostics, but with validated assays, therefore it is plausible that different panels could be used. In this sense a harmonisation process should be welcome. Reliable assays at a sustainable cost could offer a solution.
In immunotherapy, as in targeted therapy, the era of ‘one size fits all’ is past and the day-to-day work of pathologists is changing dramatically.
More and more information must be given in the same time and NGS technology is currently the only approach for this goal. In advanced solid tumours diagnosed on small biopsies and/or cytological samples, the real issue is the quantity of the specimen.
Today more than ever is ‘the tissue the issue’.
Reference
1 Kalemkerian G et al. Molecular testing guideline for the selection of patients with lung cancer for treatment with targeted tyrosine kinase inhibitors: American Society of Clinical Oncology Endorsement of the College of American Pathologists/International Association for the Study of Lung Cancer/Association for Molecular Pathology Clinical Practice Guideline Update. J Clin Oncol 2018;36:911–19.